Vision is one of the most vital senses, yet millions worldwide struggle with refractive errors that blur sight and reduce quality of life. Modern ophthalmology offers a variety of corrective options—from traditional eyeglasses and contact lenses to cutting edge refractive surgeries—that can restore clear vision. In this guide, we detail the types of refractive disorders, explain the various refractive surgical techniques available, review the necessary pre-surgical investigations, and discuss the benefits and risks associated with these procedures.
1. Refractive Disorders of the Eye
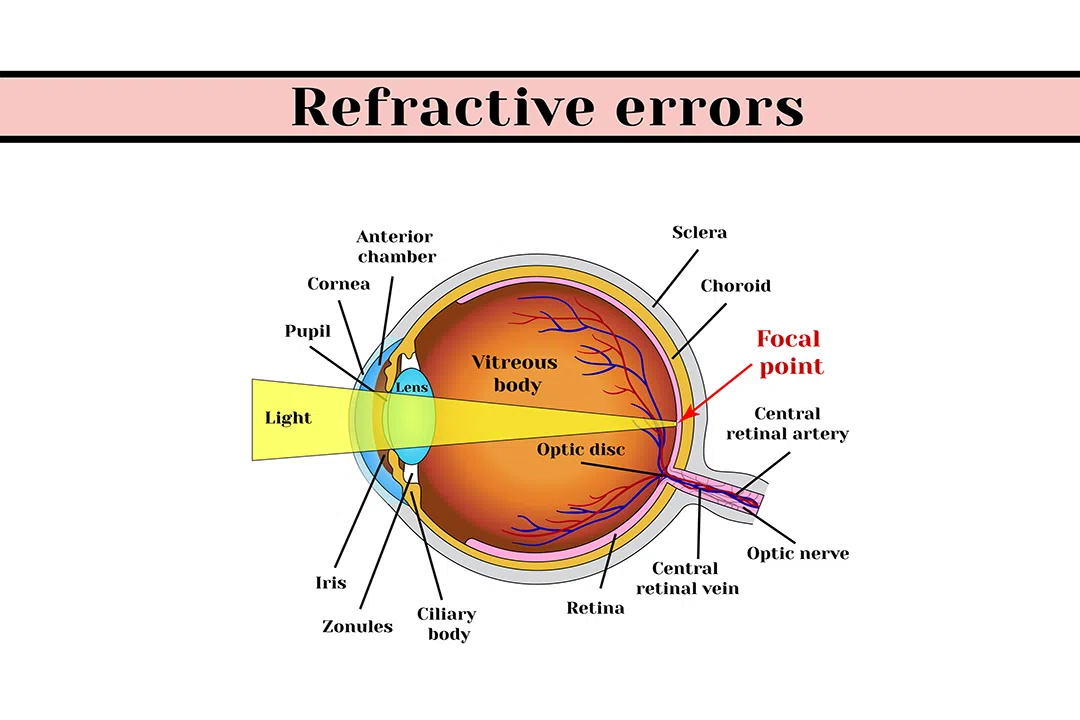
Refractive disorders occur when the optical components of the eye are unable to focus light precisely on the retina. This misalignment leads to blurred or distorted vision. The following sections outline the four primary types of refractive errors.
1.1 Myopia (Nearsightedness)
Definition and Overview
Myopia, or nearsightedness, is characterized by the clear visualization of close objects, while distant objects appear blurry. The underlying issue is that the eyeball is elongated or the cornea is excessively curved, causing light rays to converge before reaching the retina.
Causes
- Genetic Factors: A strong family history can predispose individuals to myopia.
- Environmental Influences: Extended periods of near-vision activities such as reading, computer work, or prolonged screen time, especially during childhood, can contribute to its development. Insufficient outdoor exposure has also been implicated.
Common Symptoms
- Difficulty focusing on distant objects (e.g., road signs, classroom boards).
- Frequent eye strain and headaches.
- Squinting or blinking excessively to see distant objects more clearly.
Treatment Options
- Eyeglasses or Contact Lenses: Eyeglasses and contact lenses compensate for the eye’s focal error.
- Refractive Surgery: Procedures such as LASIK, Femto Contoura LASIK, and ReLEx SMILE reshape the cornea to correct the optical pathway permanently.
1.2 Hyperopia (Farsightedness)
Definition and Overview
Hyperopia, or farsightedness, is the condition where close objects appear blurry while distant objects can often be seen more clearly. In hyperopic eyes, the eyeball is shorter or the cornea is flatter than normal, causing light to focus behind the retina.
Causes
- Genetic Predisposition: A family history of hyperopia is common.
- Anatomical Structure: The natural configuration of the eye contributes significantly to this condition.
Common Symptoms
- Difficulty reading or performing close-up tasks.
- Eye strain, particularly during prolonged near work.
- In more severe cases, even distance vision may be compromised.
Treatment Options
- Corrective Lenses: Convex (plus) lenses help converge light correctly onto the retina.
- Surgical Correction: Procedures such as LASIK and PRK can reshape the cornea to bring the focal point forward, improving near vision.
1.3 Astigmatism
Definition and Overview
Astigmatism is caused by an irregular curvature of the cornea or lens. Rather than being perfectly spherical, the surface of the cornea is more oval (or football-shaped), resulting in light being focused at multiple points. This leads to distorted or blurred vision at all distances.
Causes
- Hereditary Factors: Astigmatism often runs in families.
- Associated Eye Conditions: Chronic eye rubbing or allergic eye conditions, like allergic conjunctivitis, may worsen the irregular curvature.
- Corneal Disorders: Conditions such as keratoconus, where the cornea progressively thins and bulges, are linked to astigmatism.
Common Symptoms
- Blurred or distorted vision regardless of the viewing distance.
- Difficulties with fine detail tasks such as reading small print.
- Frequent headaches and eye fatigue as the eyes strain to correct the distortion.
Treatment Options
- Eyeglasses/Contact Lenses: Special cylindrical lenses are prescribed to correct the asymmetry.
- Refractive Surgery: LASIK, Femto Contoura LASIK, and PRK can be tailored to smooth the corneal surface and reduce the effects of astigmatism.
1.4 Presbyopia
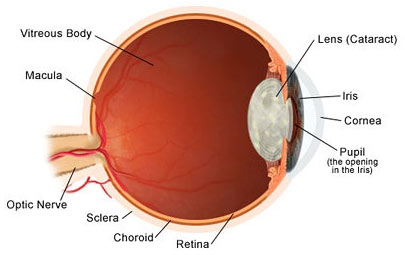
Cataract surgery Open pop-up dialog box
Definition and Overview
Presbyopia is an age-related condition in which the eye’s lens loses its elasticity, leading to diminished ability to focus on nearby objects. Unlike other refractive errors caused by the eye’s shape, presbyopia results from the natural aging process, typically emerging around the age of 40.
Causes
- Aging: The lens gradually becomes more rigid, reducing its capacity to change shape (accommodate) for near tasks.
Common Symptoms
- Difficulty reading or performing tasks that require close focus.
- The need to hold reading materials at arm’s length.
- Increased eye strain and headaches during prolonged near work.
Treatment Options
- Reading Glasses or Multifocal Lenses: Provide temporary assistance for near vision.
- Contact Lenses: Multifocal or monovision contact lenses can be used, wherein one eye is corrected for near vision and the other for distance.
- Intraocular Lenses (IOLs): In cases where presbyopia is combined with cataracts, multifocal IOLs may be implanted during cataract surgery to restore a range of vision.
2. Types of Refractive Surgeries
Refractive surgery offers a permanent solution for many refractive errors by reshaping the cornea or implanting corrective lenses. Here we discuss the most popular surgical techniques, outlining how each procedure works, its advantages, and its ideal candidates.
2.1. Femto Contoura LASIK (Bladeless LASIK)
What is Femto Contoura LASIK?
Femto Contoura LASIK is a sophisticated form of LASIK that employs a femtosecond laser to create a thin and highly precise corneal flap. This bladeless technique offers enhanced accuracy compared to traditional microkeratome-based methods.
How It Works
- Flap Creation: A femtosecond laser creates an ultra-thin, precise corneal flap.
- Customized Reshaping: An excimer laser is then used to reshape the exposed corneal tissue based on detailed topographic maps of the cornea.
- Flap Repositioning: After the corneal tissue is reshaped, the flap is repositioned, allowing for natural healing.
Key Advantages
- Precision: The bladeless approach minimizes the risk of mechanical complications.
- Enhanced Safety: Custom corneal mapping ensures that even minor irregularities are addressed.
- Rapid Visual Recovery: The precise surgical technique facilitates faster healing and reduced downtime.
Ideal Candidates
- Individuals with stable myopia, hyperopia, or astigmatism.
- Patients with healthy, adequately thick corneas.
- Those seeking minimal recovery time with a reduced risk of complications.
2.2 ReLEx SMILE (Small Incision Lenticule Extraction)
Overview
ReLEx SMILE is a minimally invasive refractive surgery primarily used to correct myopia and astigmatism. Unlike LASIK, this procedure avoids the creation of a large corneal flap, instead using a small incision to remove a precise lenticule (a small disc-shaped piece of corneal tissue).
How It Works
- Lenticule Creation: A femtosecond laser creates a lenticule within the cornea.
- Small Incision: A tiny incision (typically 2–4 mm) is made to extract the lenticule.
- Corneal Reshaping: The removal of the lenticule alters the cornea’s curvature, effectively correcting the refractive error.
Key Advantages
- Minimally Invasive: No large flap is required, which lowers the risk of flap-related complications.
- Faster Recovery: Patients often experience less discomfort and a quicker return to normal activities.
- Preservation of Corneal Integrity: The smaller incision helps maintain overall corneal strength and stability.
Ideal Candidates
- Patients primarily with myopia and mild to moderate astigmatism.
- Individuals with active lifestyles or professions where eye trauma is a risk.
- Those seeking an alternative to conventional LASIK with reduced invasiveness.
2.3 Stream Light LASIK / PRK (Photorefractive Keratectomy)
Overview
Stream Light LASIK, commonly known as PRK, is a laser-based procedure that corrects refractive errors by removing the outermost layer of the cornea (the epithelium) to expose the underlying tissue. Unlike LASIK, PRK does not involve creating a corneal flap.
How It Works
- Epithelium Removal: The superficial layer of the cornea is gently removed.
- Laser Reshaping: An excimer laser reshapes the exposed corneal tissue to correct the refractive error.
- Healing Process: The epithelium naturally regenerates over several days, with a temporary contact lens used as a bandage during the healing process.
Key Advantages
- No Flap-Related Risks: Suitable for patients with thin or irregular corneas.
- Proven Track Record: PRK has been in use for decades with well-documented safety and efficacy.
- Flexibility: Ideal for high refractive errors and patients who may not qualify for LASIK.
Ideal Candidates
- Patients with thin corneas or those at higher risk for flap complications.
- Individuals with high degrees of refractive error that may not be fully addressed by LASIK.
- Those whose lifestyles or occupations demand maximum corneal stability.
Post-Surgery Considerations
- Longer Recovery: The epithelial layer takes longer to regenerate, resulting in a longer recovery period compared to LASIK.
- Temporary Discomfort: Patients may experience pain, irritation, or light sensitivity during the healing phase.
2.4 Phakic Intraocular Lenses (IOLs)
Overview
Phakic IOLs are implantable lenses designed to correct significant refractive errors in patients who are not ideal candidates for laser-based procedures. Unlike conventional intraocular lenses used in cataract surgery, phakic IOLs are implanted without removing the eye’s natural lens.
How They Work
- Surgical Implantation: The phakic IOL is carefully inserted into the eye, typically positioned between the iris and the natural lens.
- Preservation of Natural Lens: The natural lens remains intact, preserving the eye’s ability to accommodate (change focus) naturally.
- Targeted Correction: The implant corrects high levels of myopia, hyperopia, or astigmatism that are beyond the safe correction limits of laser procedures.
Key Advantages
- Effective for Severe Errors: Provides a solution for patients with refractive errors that cannot be adequately addressed with LASIK or PRK.
- Minimal Impact on Corneal Structure: Since no corneal tissue is removed, the integrity of the cornea is preserved.
- Fast Recovery: The minimally invasive nature of the implantation facilitates a quick return to daily activities.
Ideal Candidates
- Individuals with high refractive errors who are unsuitable for laser-based procedures.
- Patients with thin or irregular corneas.
- Those seeking an alternative to conventional refractive surgery without undergoing lens removal.
Post-Surgery Considerations
- Monitoring for Cataracts: Although rare, there is a potential risk for cataract development over time.
- Regular Follow-Up: Continued eye examinations are necessary to ensure the lens remains properly positioned and the eye remains healthy.
3. Pre-Surgical Investigations
Prior to undergoing refractive surgery, a thorough eye examination and diagnostic workup are essential. These investigations help determine the patient’s suitability for the procedure and guide the customization of the treatment plan.
3.1 Detailed Eye Exam
- Visual Acuity Testing: Measures how clearly a person sees at various distances.
- Refraction Assessment: Determines the precise lens prescription necessary to correct the refractive error.
3.2 Corneal Mapping (Topography)
- Purpose: Produces a detailed map of the cornea’s surface curvature.
- Significance: Identifies irregularities such as astigmatism, corneal thinning, or keratoconus, ensuring the cornea can safely support the surgical procedure.
3.3 Pachymetry (Corneal Thickness Measurement)
- Purpose: Measures the thickness of the cornea.
- Significance: Ensures there is adequate corneal tissue for procedures like LASIK or PRK, helping to avoid post-surgical complications.
3.5 Dry Eye Testing
- Purpose: Assesses tear production and overall eye lubrication.
- Significance: Identifies patients at risk for post-surgical dry eye syndrome, allowing for preemptive management strategies.
3.6 Aberrometry (Wavefront Analysis)
- Purpose: Measures the way light waves travel through the eye, capturing subtle imperfections.
- Significance: Facilitates customized, wavefront-guided treatments to reduce higher-order aberrations like halos or glare, thus enhancing visual quality.
3.7 Eye Health History Review
- Purpose: Comprehensive review of past medical and ocular history, including previous surgeries and systemic conditions.
- Significance: Ensures that the selected surgical procedure is safe and appropriate based on the individual’s overall health profile.
4. Benefits of Refractive Surgery
Refractive surgery offers several key advantages that make it an attractive option for those seeking long-term freedom from glasses and contact lenses.
4.1 Improved Vision
- Clarity: Many patients experience significantly improved visual acuity, often reaching 20/25 vision or better.
- Long-Term Stability: Once healed, the visual improvements are generally stable, reducing the need for ongoing corrective eyewear.
4.2 Freedom from Eyewear
- Lifestyle Convenience: Eliminates the daily challenges of managing glasses or contact lenses—ideal for active individuals and professionals.
- Enhanced Aesthetics: For those who prefer not to wear glasses, refractive surgery offers a cosmetically appealing alternative.
4.3 Quick Recovery
- Minimal Downtime: Many modern procedures, such as Femto Contoura LASIK and ReLEx SMILE, allow patients to resume normal activities within 24–48 hours.
- Comfort: Advanced techniques ensure a more comfortable recovery with reduced post-operative pain and irritation.
4.4 Cost Savings Over Time
Long-Term Investment: Although the initial cost is higher than traditional corrective methods, the elimination of ongoing expenses for glasses, contacts, and lens care can yield significant savings over time.
4.5 Customized Treatment
- Tailored Corrections: Advanced diagnostic tools allow for highly personalized treatments that not only correct basic refractive errors but also address subtle visual aberrations.
- Enhanced Outcomes: Customized procedures often result in fewer visual disturbances and improved overall satisfaction.
5. Risks and Considerations of Refractive Surgery
While refractive surgery is highly effective for many patients, it is important to understand the potential risks and limitations.
5.1 Dry Eye Syndrome
- Description: Many patients experience temporary dryness and irritation following surgery.
- Management: Typically managed with artificial tears and sometimes prescription medications until normal tear production resumes.
5.2 Overcorrection or Undercorrection
- Issue: In some cases, the surgical correction may be slightly more or less than required.
- Outcome: May necessitate enhancements or additional corrective measures to fine-tune the results.
5.3 Visual Disturbances
- Symptoms: Some patients may notice halos, glare, or starbursts around lights—especially at night.
- Prognosis: These disturbances often diminish with time, though they can persist in a minority of cases.
5.4 Flap Complications (LASIK-Specific)
- Risk: In LASIK procedures, the creation of a corneal flap carries a risk of complications such as dislocation or wrinkles.
- Mitigation: Such issues are rare and can often be addressed with additional corrective procedures.
5.5 Infection and Inflammation
- Risk: As with any surgical intervention, there is a small risk of infection or post-operative inflammation.
- Prevention: Strict adherence to post-surgical care protocols and medications helps minimize this risk.
5.6 Regression of Results
- Possibility: In some cases—especially among younger patients or those with high prescriptions—the initial improvement may diminish over time.
- Solution: A follow-up or enhancement procedure may be recommended to maintain optimal vision.
5.7 Suitability for All Patients
- Consideration: Not everyone is an ideal candidate for laser-based refractive surgery.
- Alternatives: Patients with thin corneas, severe dry eye, or other ocular conditions might be better suited for procedures such as PRK, ReLEx SMILE, or phakic IOL implantation.
Conclusion
Refractive disorders, whether they affect near or far vision, can have a significant impact on everyday life. Fortunately, modern refractive surgery offers a range of tailored solutions—from advanced laser procedures to lens implants—that can dramatically improve vision. By understanding the different types of refractive errors, the surgical options available, the essential diagnostic tests, and the associated benefits and risks, patients can make informed decisions about their eye care. Always consult with a qualified eye care professional to determine the best treatment plan based on your unique needs and eye health.
Whether you’re considering refractive surgery for a more active lifestyle or simply seeking a long-term solution to dependency on glasses or contacts, the advances in eye care technology provide options that combine safety, precision, and lasting visual clarity.
FAQs
Refractive surgery is a procedure designed to correct common vision problems, such as nearsightedness (myopia), farsightedness (hyperopia), and astigmatism. The goal is to reduce or eliminate the need for glasses or contact lenses by reshaping the cornea or implanting lenses to improve how light focuses on the retina.
Ideal candidates for refractive surgery are those who:
- Are 18 years or older with a stable prescription for at least one year.
- Have healthy eyes with no major eye diseases, such as cataracts or glaucoma.
- Have sufficient corneal thickness (for LASIK and similar procedures).
- Have realistic expectations and understand the risks and benefits.
A thorough eye exam will determine your suitability for the procedure.
There are several types of refractive surgery, including:
- LASIK (Laser-Assisted in Situ Keratomileusis): A laser reshapes the cornea to correct vision. Femtosecond LASIK is a bladeless option.
- PRK (Photorefractive Keratectomy): The surface of the cornea is reshaped without creating a flap. PRK is often recommended for patients with thin corneas.
- ReLEx SMILE (Small Incision Lenticule Extraction): A minimally invasive laser procedure that reshapes the cornea through a small incision.
- Femto Contoura LASIK: A customized LASIK procedure using advanced topography-guided laser technology for improved precision.
- Phakic IOLs (Intraocular Lenses): For patients with high refractive errors who may not be candidates for LASIK or PRK, phakic lenses are implanted inside the eye to correct vision.
Most patients report minimal discomfort during the procedure. LASIK and ReLEx SMILE are generally painless, though you may feel mild pressure during the laser application. After surgery, some temporary discomfort (like dryness, itching, or a sensation of something in the eye) is common but usually resolves within a few hours to days.
Recovery times vary depending on the procedure:
- LASIK: Most people notice improved vision within 24 to 48 hours, with full recovery taking 1-2 weeks.
- PRK: Since the surface layer of the cornea needs to heal, recovery may take 3-7 days for initial healing, with full stabilization taking several weeks.
- ReLEx SMILE: Similar to LASIK, most patients experience rapid vision improvement within 24-48 hours, with full recovery in 1-2 weeks.
