The retina layer sits at the innermost boundary of the eye and lines the back of the eyeball. This remarkable tissue converts light into neural signals. A mere 0.5mm thick, it works like a natural image processor that turns photons into electrical impulses. These signals travel to the brain and help us recognize what we see.
Retina eye function and structure explained
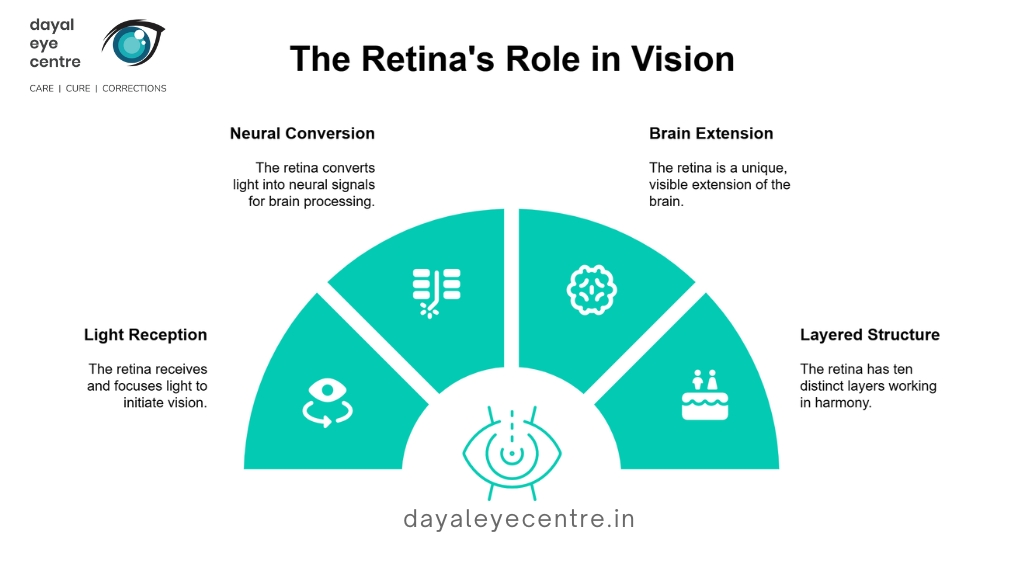
The retina’s main job is simple – it receives focused light, converts it to neural signals, and sends them to the brain. The retina stands out as unique because it’s actually an extension of the brain. Scientists find this fascinating because it’s the only brain tissue we can see from outside the body.
The retina has ten distinct layers that work together in perfect harmony:
- Inner limiting membrane
- Nerve fiber layer
- Ganglion cell layer
- Inner plexiform layer
- Inner nuclear layer
- Middle limiting membrane
- Outer plexiform layer
- Outer nuclear layer
- External limiting membrane
- Layer of rods and cones
These layers combine their efforts to process visual information. Six main cell types make up the retina: rods, cones, retinal ganglion cells, bipolar cells, horizontal cells, and amacrine cells. Each cell type plays its own special role in creating vision.
The retina uses oxygen faster than any other tissue in our body. It has a specialized dual blood supply to meet these extraordinary energy needs.
Photoreceptor cells and signal transmission
Light processing happens through the retina’s photoreceptor cells – rods and cones. Our eyes have about 6 million cones and an amazing 120 million rods. Rods dominate the outer retina and help us see in dim light (scotopic vision). Cones cluster in the center and handle color and detail in bright conditions (photopic vision).
We have three types of cones – red light sensitive (64%), green light sensitive (32%), and blue light sensitive (2%). The fovea, which sits at the retina’s center, contains only cones. This gives us our sharpest vision. Rods stay away from the fovea but become more numerous toward the retina’s edges.
The sort of thing i love about phototransduction is how it changes light into neural signals. The process follows an intricate sequence. Photoreceptors catch light using photopigments like rhodopsin, which sets off a chain reaction:
- Light alters the retinal’s shape in the photoreceptor
- This wakes up a G-protein called transducin
- Transducin activates an enzyme (phosphodiesterase)
- The cell then becomes hyperpolarized as channels close
- This changes how neurotransmitters get released
- Signals move through bipolar cells to ganglion cells
- Ganglion cells send these signals to the brain through the optic nerve
Why the retina is critical for vision
We just need healthy retinas to see. This delicate tissue serves as our primary visual processor. Any damage often leads to permanent vision loss.
The retina works as our original filter and analyzer of visual information. Its neural networks do substantial processing before sending signals to the brain. They split details about motion, color, form and contrast into separate pathways.
Special circuits in the retina detect specific visual features. They start analyzing what we see before the information leaves our eyes. To cite an instance, see how some retinal cells respond only to moving objects, while others focus on contrasts or colors.
The retina’s processing splits visual information into two main pathways. The magnocellular pathway handles motion and changes, while the parvocellular pathway processes shape and color. This dual processing system makes human vision incredibly complex.
The retina’s complex development and high energy needs make it vulnerable to many diseases that can harm vision. Regular eye checkups help protect retinal health and maintain good vision throughout life.
Common Retina Diseases and Their Causes
The retina can develop several serious conditions that lead to vision loss or blindness without treatment. Early detection and treatment depend on understanding these diseases and what causes them.
Retinal tear and detachment
Retinal detachment happens when the retina separates from the eye’s supporting tissues. This dangerous condition comes in three main forms. The most common type, rhegmatogenous detachment, starts when fluid collects behind the retina through a small tear. Scar tissue can pull the retina away and cause tractional detachment, which often affects people with diabetes. The third type, exudative detachment, occurs when fluid builds up without any tears.
People face higher risks if they’re older, have had eye surgery, suffered eye injuries, or are very nearsighted. Young males account for about 10% of retinal detachments from blunt trauma. Each year, 6.3 to 17.9 people per 100,000 develop rhegmatogenous retinal detachment. Vision loss becomes permanent within days without quick treatment.
Diabetic retinopathy and hypertension effects
High blood sugar damages the retina’s blood vessels and leads to diabetic retinopathy. The blood vessels start to weaken and develop small bulges that leak. This condition gets worse over time, moving from early (nonproliferative) to advanced (proliferative) stages. New abnormal blood vessels grow in advanced cases and often cause vitreous hemorrhage or retinal detachment.
The retina also suffers when blood pressure stays high for too long, causing hypertensive retinopathy. Research shows 4% to 18.7% of adults without diabetes have this condition. Blood vessels in the retina become tight and stiff from high pressure, which reduces blood flow. These changes often warn doctors about possible heart problems.
Macular degeneration and macular hole
AMD affects central vision as people age. Dry AMD makes up about 90% of cases. It starts when protein deposits called drusen form under the macula and make it thinner. Wet AMD moves faster and causes more vision loss because abnormal blood vessels grow and leak under the retina. AMD affects almost 20 million Americans and ranks as a top cause of vision loss in people over 60.
A macular hole forms differently. The eye’s vitreous gel shrinks with age and pulls away from the retina, sometimes creating a hole in the macula. About one in ten people who get a macular hole in one eye will develop it in their other eye too.
Retinitis pigmentosa and genetic conditions
Retinitis pigmentosa (RP) has several inherited disorders that cause vision to get worse over time. This rare condition affects one in 3,000-7,000 people. Night blindness comes first, followed by loss of side vision. Scientists have found more than 40 genes that cause RP, with different mutations creating various inheritance patterns.
RP occurs with other non-eye diseases in 20-30% of patients. The inheritance breaks down into autosomal dominant (20-25%), autosomal recessive (15-20%), X-linked recessive (10-15%), and random cases (30%). The outlook isn’t all bad – 52% of RP patients over 45 can still see at 20/40 or better.
Retinal vein occlusion and eye trauma
Blood clots can block veins that drain blood from the retina, causing retinal vein occlusion. The blockage can affect either the main vein (central) or smaller branches. More than 16 million people worldwide have this condition. Sometimes arteries harden and press against retinal veins, which disrupts blood flow and creates clots.
Eye injuries pose another serious threat to the retina. Sports accidents, crashes, or explosions can tear or detach the retina right away. Quick movements during car accidents can damage the retina even without direct hits. People over 40 and those with diabetes or high blood pressure face much higher risks for these retinal problems.
Recognizing Retina Damage Symptoms Early
Your vision depends on catching retinal damage early. Quick action when you notice warning signs can save your sight before conditions get worse.
Flashes of light and floaters
You should pay attention to sudden flashes of light that look like lightning streaks, sparkles, or camera flashes. These light shows happen when the vitreous gel pulls or rubs against your retina. This could mean you have a retinal tear. Dark specks, threads, or cobwebs might drift across your vision too. A few floaters are normal as you age, but you should worry if many new ones appear suddenly.
Your retina might be detaching if you see a “shower” of new floaters with flashes – this needs emergency medical care right away. You might see these flashes and floaters together or on their own. They stand out most against bright surfaces like white paper or blue sky.
Blurred or distorted central vision
Straight lines that look wavy or irregular point to problems with your macula. This could be age-related macular degeneration or macular holes. Your central vision might blur slowly or suddenly based on what’s causing it.
You might still see things on the sides clearly, but damage to your macula makes daily tasks harder. Reading becomes difficult. You might struggle to recognize faces or drive safely.
Sudden loss of peripheral vision
Losing side vision creates a tunnel effect. You see what’s straight ahead but miss objects on the sides unless you turn your head. This affects about 13% of people over 65 and limits their independence.
Watch out for shadows that move across your vision like a curtain – your retina might be detaching. In fact, sudden side vision loss could mean you’re having a stroke, especially if one side of your body feels weak.
Difficulty adjusting to light changes
Your retina’s light sensors might be damaged if you struggle to see when moving between bright and dark places. Night blindness shows up early in conditions like retinitis pigmentosa, where rod cells break down over time.
Get emergency care right away if you notice:
- You suddenly can’t see in one or both eyes
- New floaters with flashes of light appear
- A curtain-like shadow moves across your vision
- Your side vision changes suddenly
Don’t skip regular eye checkups. Many retinal problems don’t show early symptoms, so doctors can catch them before permanent damage sets in.
Retina Test and Diagnosis Procedures
Eye doctors use specialized testing methods to diagnose retinal conditions. These tests help them see and analyze the retina in detail. Doctors can identify problems early before symptoms become severe.
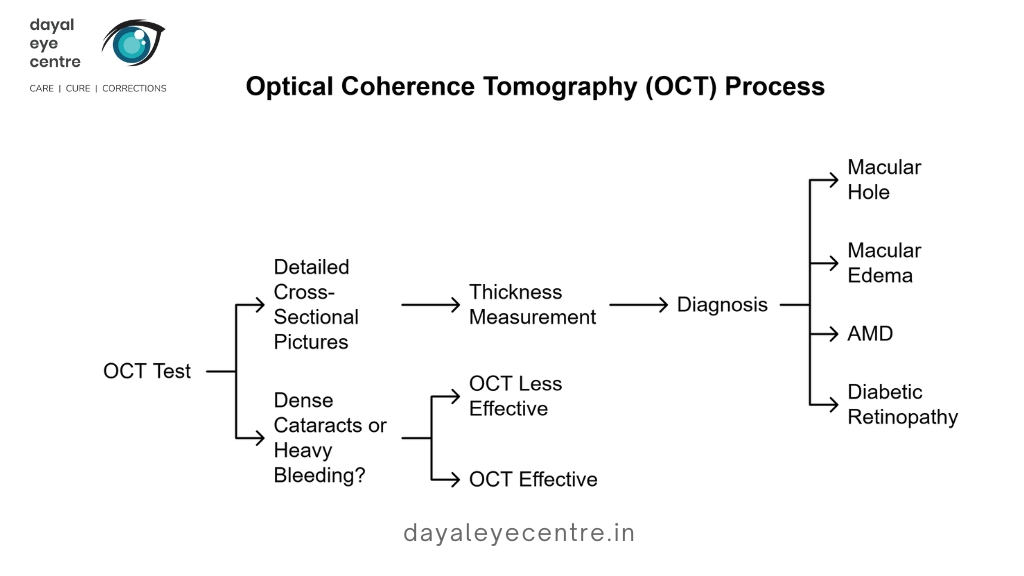
Optical coherence tomography (OCT)
OCT creates detailed cross-sectional pictures of your retina with light waves without any invasive procedures. Doctors can view and measure the thickness of each unique retinal layer. The test is quick, taking just a few minutes with no special preparation needed. OCT helps diagnose many conditions like macular holes, macular edema, age-related macular degeneration, and diabetic retinopathy. Dense cataracts or heavy bleeding can block light from passing through the eye, making OCT less effective.
Fluorescein and indocyanine green angiography
These imaging tests use dyes injected into your arm’s vein to highlight retinal blood vessels. We used fluorescein angiography to see retinal circulation. Indocyanine green angiography (ICGA) shows better images of choroidal vasculature. ICGA works great especially when you have blood, fluid, or pigment blocking other imaging methods. These tests help detect unusual blood vessel growth, leaks, or blockages in retinal conditions of all types.
Amsler grid and fundus autofluorescence
The Amsler grid offers a simple but powerful way to detect vision distortions. Patients can monitor changes in their central vision at home using this square-shaped graph with uniform lines. Fundus autofluorescence (FAF) creates maps of natural fluorophores in the retina, mostly from lipofuscin in retinal pigment epithelium cells. This technique reveals important details about retinal health and disease progression that other methods might miss.
Ultrasound and MRI for deeper analysis
Ultrasound provides a safe way to examine eye structures when doctors can’t see the retina directly. B-scan ultrasound creates two-dimensional cross-sectional images to detect retinal detachments, vitreous hemorrhages, and tumors. MRI shows complete images of the eye and surrounding structures. It provides detailed anatomical and functional information even through cloudy areas.
Retina Treatment Options and Surgical Methods
Different retinal conditions need specific treatment approaches. Modern eye doctors now have several ways to save vision if they catch problems early enough.
Laser photocoagulation and cryopexy
Doctors use laser photocoagulation to create tiny burns that seal tears in the retina or destroy abnormal blood vessels. This treatment slows blood vessel leakage in diabetic retinopathy and reduces vision loss risk by over 50% at 12 months. The procedure takes about 15 minutes in a doctor’s office. Patients might see temporary flashes of light during the treatment.
Cryopexy uses extreme cold to freeze the retina around tears. The freezing creates scar tissue that connects the retina to tissue underneath, which stops detachment. Eye doctors often choose cryopexy for tears in the outer retina or when lasers can’t reach certain areas.
Vitrectomy and scleral buckle surgery
A vitrectomy removes some or all of the eye’s vitreous gel to reach the retina. The surgeon makes small cuts in the sclera, takes out the cloudy vitreous, fixes retinal damage, and puts in saline, gas, or silicone oil instead. This surgery helps patients with diabetic retinopathy, retinal detachment, macular holes, and serious eye injuries.
Scleral buckling uses a silicone band around the eye’s outer part. This creates an indent that pushes the loose retina back where it belongs. The success rate reaches 80-90% based on recent studies. Doctors sometimes combine both procedures to fix complex retinal detachments.
Anti-VEGF injections and retina eye drops
Anti-VEGF medications have transformed retinal care by stopping abnormal blood vessels from growing. These shots help stabilize vision in 90% of patients and improve sight in 30%. Patients can receive Beovu (brolucizumab), Avastin (bevacizumab), Lucentis (ranibizumab), Eylea (aflibercept), or Mucugen (pegaptanib sodium).
New research shows promise in retina eye drops that could replace injections. Studies found drops with caspase-9 inhibitors worked twice as well as regular injections. These drops reduced swelling and improved blood flow in mice with retinal vein occlusion.
Retinal prosthesis for severe vision loss
Retinal prostheses (“bionic eyes”) give basic sight back to people who have lost most of their vision. These devices help patients with retinitis pigmentosa and age-related macular degeneration. Doctors have implanted these devices in more than 500 patients worldwide in the last 15 years.
The prostheses come in three types: epiretinal (on the retina), subretinal (under the retina), and suprachoroidal. These devices have limits but help patients find high-contrast objects, move around, and do basic tasks.
Conclusion
The retina’s role extends beyond scientific interest – it affects how well we protect our eyesight throughout our lives. This delicate tissue layer’s amazing complexity makes it prone to many disorders that can harm vision permanently. Your best chance at successful treatment comes from catching problems early through regular checkups.
Never ignore warning signs like sudden floaters, light flashes, or changes in side vision. These symptoms often point to serious conditions that need a doctor’s care right away. Everyone needs detailed eye exams regularly, especially when you have risk factors like diabetes, high blood pressure, or retinal problems running in your family.
Treatment choices have grown by a lot over recent decades. Doctors now use lasers, surgery, and injectable medicines to treat conditions that once had no cure. New technologies like retinal implants also show promise for patients who have lost much of their vision.
Your retinal health needs careful attention. Quick treatment versus waiting could save your precious eyesight. Make regular checkups with qualified eye doctors a priority. The way you care for your eyes today shapes how well you’ll see tomorrow.
FAQs
-
What are the early warning signs of retinal problems?
Early symptoms include sudden flashes of light, an increase in floaters, blurred or distorted central vision, sudden loss of peripheral vision, and difficulty adjusting between bright and dim environments. If you experience any of these symptoms, seek immediate medical attention.
-
How is retinal detachment treated?
Treatment for retinal detachment typically involves surgical procedures such as laser photocoagulation, cryopexy, pneumatic retinopexy, scleral buckling, or vitrectomy. The specific treatment depends on the type and severity of the detachment, and prompt intervention is crucial to prevent permanent vision loss.
-
Can diabetic retinopathy be prevented?
While not entirely preventable, the risk of diabetic retinopathy can be significantly reduced by maintaining good blood sugar control, managing blood pressure, having regular eye exams, and following a healthy lifestyle. Early detection and treatment are key to preventing vision loss.
-
What is age-related macular degeneration (AMD) and how is it managed?
AMD is a condition affecting the central part of the retina called the macula, primarily in older adults. Management may include anti-VEGF injections, laser therapy, and nutritional supplements. Regular eye check-ups are essential for early detection and treatment.
-
Are there any new treatments for severe retinal diseases?
Emerging treatments include retinal prostheses or "bionic eyes" for patients with profound vision loss due to conditions like retinitis pigmentosa. Additionally, researchers are developing eye drops that may replace injections for some retinal conditions, offering less invasive treatment options in the future.