Phakic intraocular lenses work like internal contact lenses that stay in your eye permanently. Your natural lens helps us see clearly, much like a camera lens. When vision problems occur, these specialized implants correct your vision without removing your eye’s original lens. This preservation gives phakic lenses their name – “phakic” means keeping your natural lens intact.
Phakic lens placement in front of natural lens
Doctors place these lenses in one of two positions, depending on your specific eye anatomy. Think of them as working either in front of or behind the colored part of your eye.
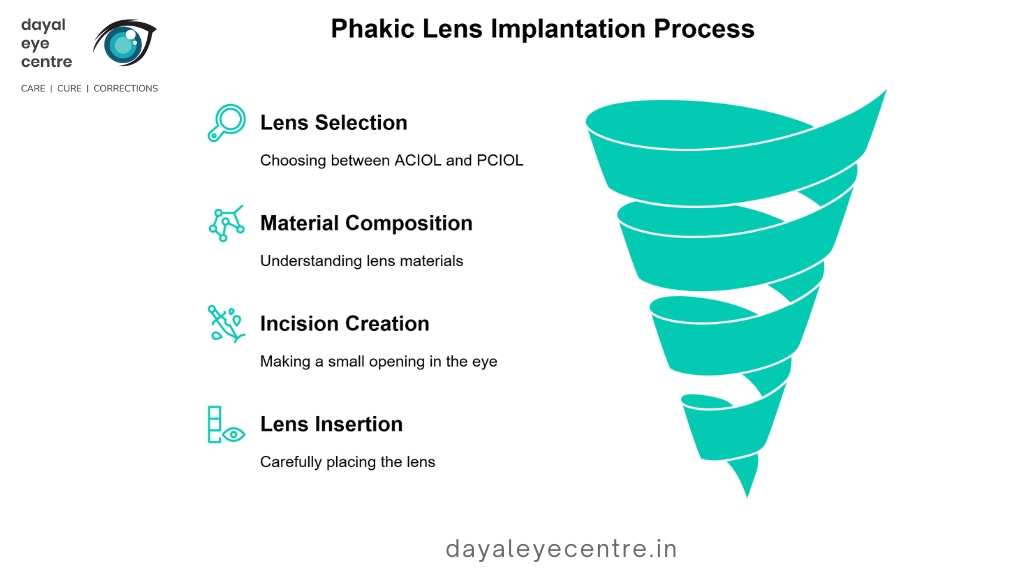
Phakic IOLs come in two main types:
- Anterior Chamber IOLs (ACIOLs) – Positioned in front of your iris (the colored part of your eye), with two variations:
- Angle-supported designs that rest in the anterior chamber angle
- Iris-fixated designs that attach to the iris using a clip mechanism
- Posterior Chamber IOLs (PCIOLs) – Implanted behind your iris but in front of your natural lens
The FDA has approved specific models from both categories for use in the United States. The Verisyse (an iris-claw ACIOL) and the Visian ICL (a PCIOL) have received official clearance. The Visian ICL features an innovative design with a 360-micron diameter central port allowing natural fluid flow, eliminating the need for additional procedures before implantation.
These lenses use different materials depending on the manufacturer. The Visian ICL contains “collamer,” a special material combining hydroxyethyl methacrylate and porcine collagen. This biocompatible composition reduces rejection risks. Other models use medical-grade plastic or silicone.
During your procedure, the surgeon creates a small incision in the front of your eye – like opening a tiny door. Through this opening, your doctor carefully inserts the phakic lens and positions it either in front of or behind your iris. The entire process typically takes about 30 minutes.
How it corrects myopia by refocusing light on the retina
To understand how these lenses help your vision, picture how a camera works. In normal vision, light rays focus precisely on your retina, creating clear images. However, with nearsightedness, these light rays focus at a point in front of your retina instead. This incorrect focusing makes distant objects appear blurry.
Phakic lenses redirect light properly within your eye. They ensure the focal point lands exactly on your retina rather than in front of it. This correction gives you clearer distance vision without glasses or contacts.
The results speak for themselves. FDA trials of iris-fixated pIOLs showed uncorrected visual acuity of 20/40 or better in 84% of patients and 20/20 or better in 31% after three years. Similarly, posterior chamber pIOLs delivered 20/40 or better vision in 81% of patients and 20/20 or better in 41%.
What makes these lenses truly valuable? They correct severe nearsightedness that laser procedures simply cannot address. Phakic lenses effectively treat myopia up to -20 diopters with excellent results. For patients with extreme nearsightedness, this offers a solution where other options fail.
Studies show phakic IOLs provide better visual outcomes for highly myopic eyes compared to LASIK and other laser procedures. They also avoid risks associated with removing corneal tissue.
The beauty of this approach lies in how these lenses work with your eye’s natural structures. Because your natural lens stays untouched, your eye keeps its focusing ability – that natural power that helps you adjust between near and far objects. This preservation gives phakic lenses a major advantage over procedures that remove or replace your natural lens.
Who is a Good Candidate for Phakic Eye Surgery?
Talk with your eye doctor about whether phakic eye surgery might work for you. Like any other procedure in the body, phakic lens implantation requires specific conditions for best results. Your eligibility depends on several key factors that help ensure both safety and effectiveness.
Age and vision stability requirements
The ideal age range for phakic lens candidates falls between 21 and 45 years. This timeline represents when your eyes have fully developed but haven’t yet begun experiencing significant age-related changes. Though the FDA hasn’t approved these lenses for people under 21, some special cases might still benefit from the procedure.
Your prescription needs to remain stable before considering surgery. Most doctors look for less than 0.5 diopters of change over at least one year. Shifting vision could signal underlying issues that might affect your surgical outcome. If you’re pregnant, breastfeeding, or managing conditions like diabetes, discuss these factors with your eye doctor, as they may increase certain risks.
Beyond age and stable vision, your eyes must meet specific anatomical requirements:
- Sufficient anterior chamber depth to safely fit the lens
- Healthy endothelial cell count (minimum varies by lens type)
- Normal iris and pupil structure
- Clear natural lens without cataracts
Your general health matters too. Certain conditions – particularly autoimmune diseases like lupus or rheumatoid arthritis – might interfere with proper healing. Some medications, including retinoic acid and steroids, could potentially compromise your recovery.
Why some patients are not eligible for LASIK
About 20-25% of patients seeking vision correction don’t qualify for LASIK, yet many of these individuals make excellent candidates for phakic IOLs. The good news? Phakic lenses often provide solutions when LASIK isn’t an option.
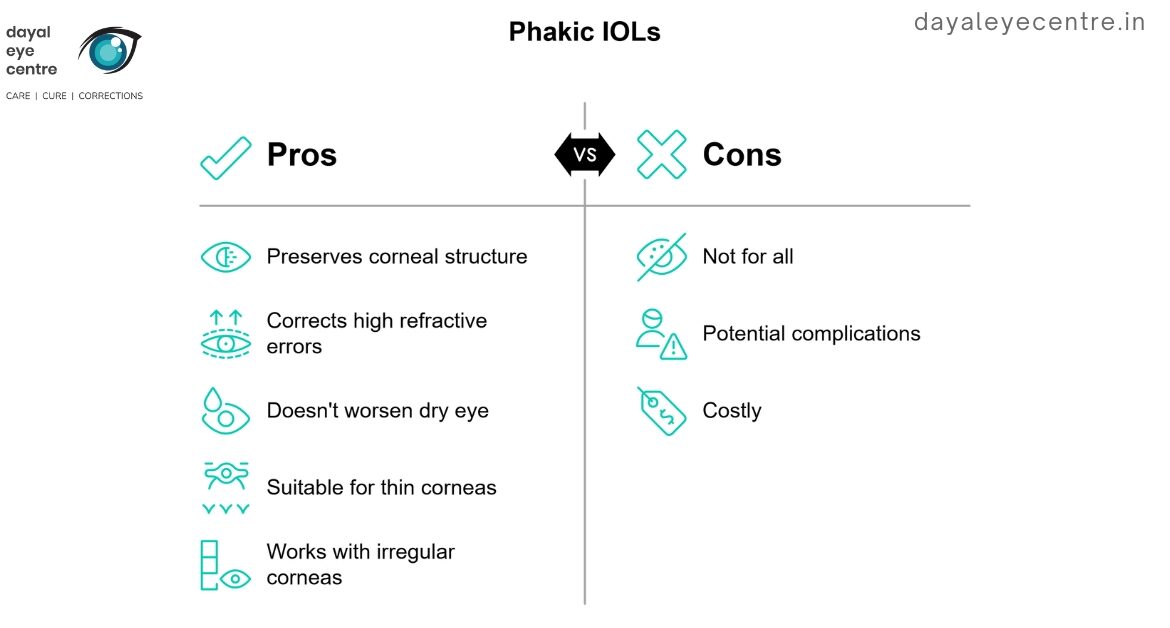
Corneal thickness presents a major limiting factor for LASIK. The procedure works by removing corneal tissue to reshape your eye, but if you have naturally thin corneas, you might lack sufficient tissue for safe removal. Phakic IOLs preserve your corneal structure entirely.
Irregular corneal topography – including conditions like keratoconus – often disqualifies patients from LASIK. Phakic lenses can work well for patients with stable keratoconus who have undergone corneal cross-linking.
High refractive errors beyond LASIK’s corrective range represent another reason to consider phakic lenses. If your myopia exceeds -8 diopters, phakic IOLs typically offer better results. At these extreme levels of nearsightedness, LASIK would require removing too much corneal tissue, potentially compromising eye stability.
For those prone to dry eye syndrome, phakic lenses offer another advantage. Since the procedure doesn’t alter your cornea or affect tear ducts, it typically doesn’t worsen dry eye symptoms like LASIK might.
Though phakic IOLs help many patients ineligible for LASIK, not everyone qualifies. You might not be a candidate if you have:
- Chronic eye inflammation (uveitis)
- Cataracts
- Significant retinal problems
- Angle abnormalities
- Glaucoma or high eye pressure
Before considering phakic eye surgery, schedule a comprehensive examination to assess all eligibility factors and establish realistic expectations about outcomes and potential risks.
Benefits of Phakic Intraocular Lenses
Talk with your eye doctor about the exceptional advantages phakic lenses offer compared to standard vision correction options. For patients with extreme nearsightedness, these specialized implants provide solutions when other procedures simply can’t help.
High myopia correction beyond LASIK limits
Phakic lenses correct severe nearsightedness that exceeds what LASIK can safely treat. While LASIK typically stops around -8 diopters (depending on your corneal thickness), phakic IOLs effectively correct myopia up to an impressive -20 diopters with excellent visual outcomes. This expanded range brings hope to patients previously told their vision was “too poor” for surgical correction.
The superiority of phakic lenses for extreme myopia isn’t just about treating higher prescriptions – it’s about quality of vision. Clinical data shows phakic IOL implantation helps most patients achieve uncorrected visual acuity better than 20/40. In fact, studies involving Visian ICL found that 84.7% of eyes achieved vision within 1.0 D of predicted refraction one year after surgery.
Unlike LASIK, which permanently removes corneal tissue, phakic IOLs work without altering your corneal shape. This preservation of your eye’s natural architecture significantly reduces risks associated with corneal thinning and potential ectasia. Your cornea maintains its structural integrity, an important factor for long-term eye health.
Preservation of natural lens and accommodation
The most significant advantage of phakic IOLs comes from keeping your natural lens intact. Like any other procedure in the body, phakic lens surgery respects your eye’s natural anatomy. By preserving your crystalline lens, these implants maintain your eye’s accommodative function – your ability to focus at different distances. This benefit proves especially valuable if you’re between 20-40 years old and still rely on this focusing power for reading and other near vision tasks.
In contrast, procedures that remove your natural lens (like refractive lens exchange) sacrifice this focusing capability completely. Professor Thomas Kohnen, who has implanted more than 2,500 phakic lenses, notes: “Phakic IOLs offer a lot of advantages… it is the only reversible procedure, and also one where we don’t experience problems with postoperative power calculations because we are not changing the cornea.”
The good news? Keeping your natural lens intact may also reduce the risk of retinal detachment often associated with lens replacement procedures. Your visual quality typically surpasses what’s possible with other techniques that alter your eye’s fundamental structure.
Reversibility and biocompatibility
Perhaps the most comforting aspect of phakic IOLs is their reversibility. Unlike laser procedures that permanently alter eye structure, your doctor can remove or replace phakic lenses if needed. This feature provides reassurance if you’re concerned about committing to permanent vision changes or want to keep options open for future vision correction technologies.
Modern phakic lenses feature materials specifically designed for maximum compatibility with your eye. The Visian ICL, currently the only FDA-approved posterior chamber phakic IOL in the United States, uses “collamer” – a copolymer containing hydroxyethyl methacrylate and porcine collagen. This advanced biocompatible material contains purified collagen that prevents adverse immune responses.
Newer designs like the EVO ICL feature a central port allowing natural fluid circulation through your eye, substantially reducing complication risks compared to earlier models. This innovation eliminates the need for preoperative laser iridotomies that were once standard practice.
Phakic IOLs offer a unique combination of benefits: exceptional vision correction for extreme nearsightedness, preservation of your eye’s natural focusing ability, and the peace of mind that comes with a reversible procedure using biocompatible materials. Talk with your eye doctor about whether these advantages make phakic lenses the right choice for your vision needs.
What to Expect During and After Surgery
Understanding your phakic lens surgery journey helps you prepare properly for each step. Like any other procedure in the body, phakic eye surgery follows distinct phases from preparation through recovery. Most patients find the process more comfortable than expected.
Surgical steps and anesthesia used
Your phakic lens procedure takes just 15-30 minutes with minimal discomfort. Most eye surgeons perform this as an outpatient procedure using numbing eye drops. If you feel anxious about the surgery, your doctor may offer a mild sedative to help you relax. In rare situations, local anesthetics around the eye or general anesthesia might be used.
Before beginning, your surgeon dilates your pupil and cleans the eye area. The key step involves creating a small incision in your cornea – where the clear front surface meets the white part of your eye. Through this tiny opening, your surgeon carefully positions the phakic lens either in front of or behind your iris, depending on the lens type. The incision usually seals itself, rarely needing stitches.
If you wear contact lenses, you’ll need to stop using them temporarily before surgery:
- Soft contacts: Remove at least one week before
- Rigid lenses: Stop wearing two weeks prior
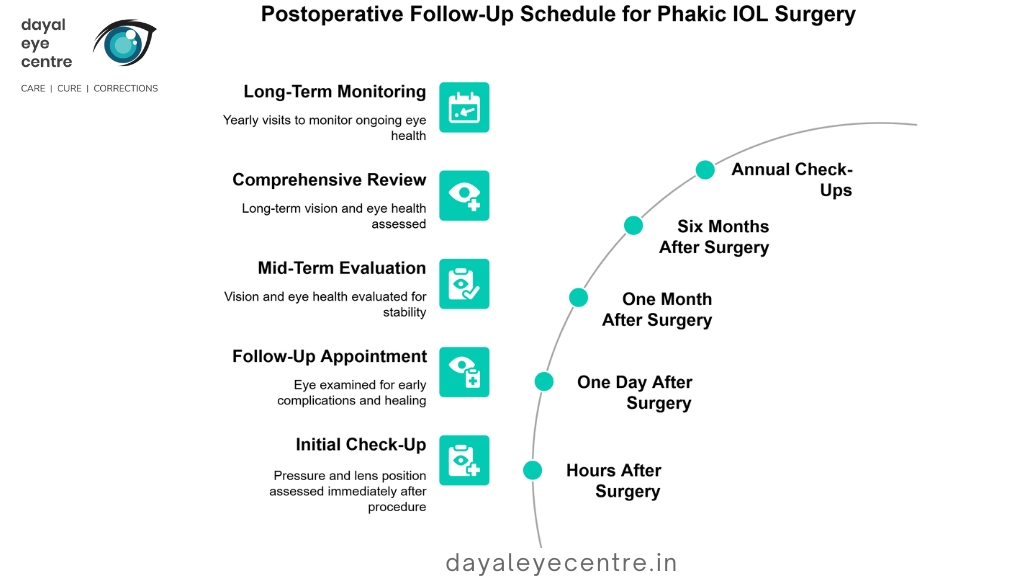
Recovery timeline and follow-up visits
Your vision will be blurry right after the procedure, similar to looking through a foggy window. Your doctor will cover your eye with a protective shield initially. Though vision starts clearing within days, you cannot drive immediately after surgery.
Most patients return to normal activities within 2-3 days, though complete healing takes about eight weeks. Your follow-up schedule typically includes:
- First check-up: Hours after surgery to check pressure and lens position
- Second appointment: One day after the procedure
- Additional visits: At one month and six months
- Long-term care: Annual check-ups to monitor eye health
While most patients see improvement quickly, full vision stabilization takes 2-4 weeks. Your doctor will track your progress during these important follow-up visits.
Postoperative care and eye drop regimen
Take comfort knowing that proper care dramatically improves your outcomes. Your surgeon will prescribe antibiotic and anti-inflammatory eye drops to prevent infection and reduce inflammation. These medications typically continue for several weeks following a specific schedule.
For the best recovery results:
- Keep your hands away from your eyes, especially during the first 3-5 days
- Wear protective eyewear while sleeping for the first week
- Avoid heavy lifting or bending for 4-7 days
- Stay away from swimming pools for at least one month
- When using digital devices, follow the 20-20-20 rule: every 20 minutes, look at something 20 feet away for 20 seconds
When applying your eye drops, always wash your hands thoroughly first. Avoid touching the dropper tip to your eye or eyelashes. Wait approximately five minutes between different medications.
Contact your doctor immediately if you experience severe pain, as this could indicate a complication requiring prompt attention. Most patients experience only mild discomfort that resolves quickly with proper medication.
Risks and Complications to Be Aware Of
Like any other procedure in the body, phakic lens implantation carries some potential risks. Though complications remain uncommon, understanding these possibilities helps you make an informed decision about your vision correction options.
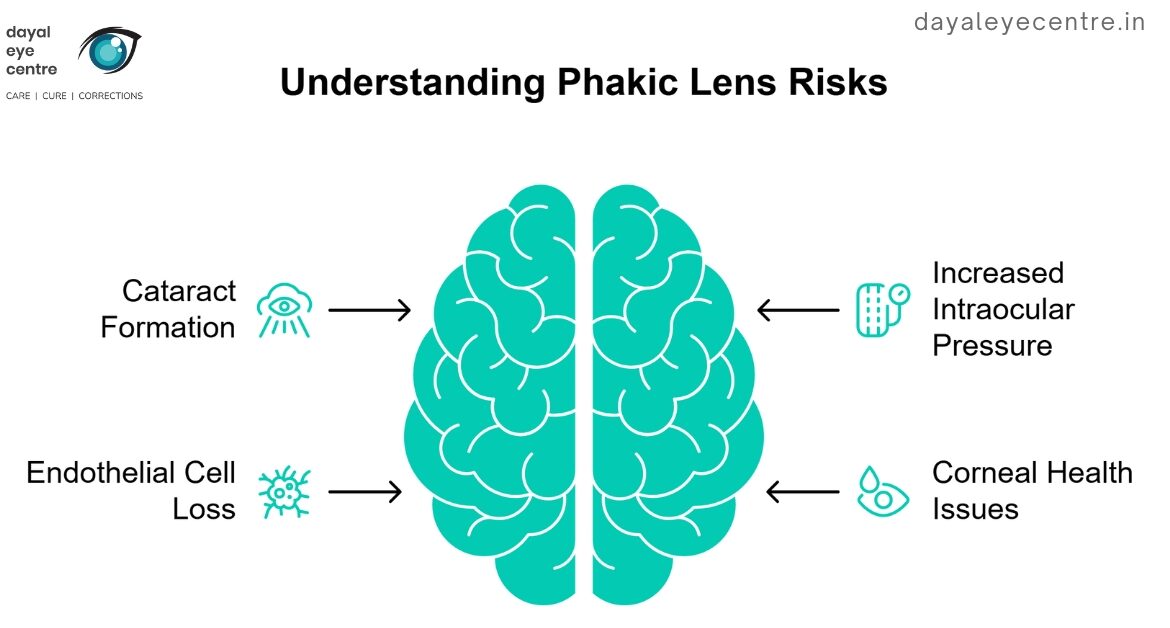
Cataract formation and lens touch
Cataracts develop in about 3.72% of patients overall following phakic IOL placement. The numbers show different risks depending on lens type – posterior chamber phakic IOLs have a higher rate (7.25%) compared to anterior chamber (1.36%) and iris-fixated lenses (1.16%). For patients with low lens vaulting, this risk jumps dramatically, with cataracts forming in 30.8% of these eyes.
Your risk increases with certain factors [link_18]:
- Age over 45 years
- Nearsightedness greater than -14.00 diopters
- Central vaulting less than 52 μm
Early cataract formation typically comes from surgical trauma, while later cataracts often develop from direct contact between the phakic IOL and your natural lens. Precise lens sizing remains critical for preventing this complication.
Increased intraocular pressure and glaucoma
About 5-10% of patients experience elevated eye pressure after receiving phakic IOLs [link_19]. A detailed study found pressure spikes in 10.8% of eyes after ICL implantation. These pressure increases typically happen either the first day after surgery (39.7% of cases) or between 2-4 weeks later (37.9%).
The main causes include:
- Retained viscoelastic material (most common immediate cause)
- Response to steroid eye drops (most frequent delayed cause)
- High ICL vault creating pupillary block (10.3% of cases)
- Synechial angle closure (6.9%)
Even with proper treatment, about 8.6% of patients with elevated pressure need to continue glaucoma medications long-term. Regular pressure checks during follow-up visits help catch and manage this issue early.
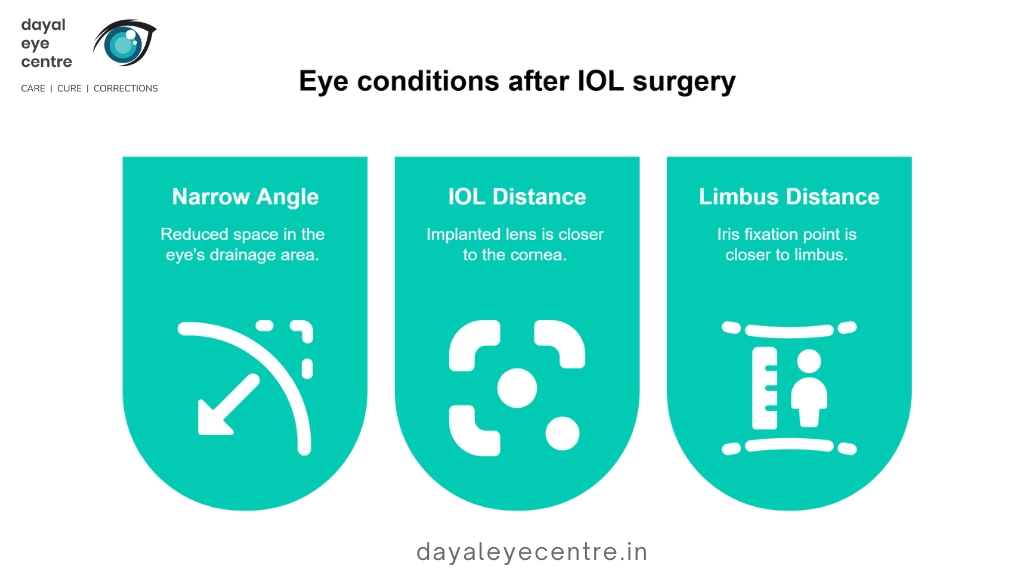
Endothelial cell loss and corneal health
The most serious long-term concern involves corneal endothelial cell loss. Your corneal cells naturally decrease by about 0.6% yearly as you age. After phakic IOL placement, this rate may increase to 1-3% per year.
The American Academy of Ophthalmology recommends removing phakic IOLs when cell loss reaches 25% after three years. Studies show this threshold occurs in 1-3% of eyes with Artisan/Verisyse lenses and 3% with Artiflex implants.
Your risk for faster cell loss increases with:
- Smaller anterior chamber angle
- Shorter distance between the IOL and your cornea
- Shorter distance from limbus to iris fixation
To protect your corneal health, you’ll need regular cell count measurements throughout the life of your phakic lenses. These check-ups help your doctor monitor your eye health and address any concerns promptly.
Talk with your eye doctor about these potential risks and how they apply to your specific situation. Understanding both benefits and possible complications helps you make the best choice for your vision needs.
FAQs About Phakic IOLs
Patients considering phakic lenses often ask similar questions during consultations. Understanding these common concerns helps you make an informed decision about whether this procedure might be right for your vision needs.
Can the lens be removed later?
Yes, phakic lenses offer excellent reversibility. Though the FDA states these lenses are “intended to be permanent,” they explicitly acknowledge the lenses “can be surgically removed” if needed. Talk with your eye doctor about this reassuring aspect of phakic IOLs.
The good news? The removal procedure remains straightforward. Because phakic lenses are thin and flexible, your surgeon can extract them through standard 2.75 mm incisions. In one documented case, a patient benefited from a phakic IOL for 10 years before removal when an anterior cataract developed.
Like any other procedure in the body, removal comes with certain considerations. The FDA notes that “return to your previous level of vision or condition of your eye cannot be guaranteed” after lens removal. However, this reversibility provides peace of mind for many patients concerned about committing to permanent vision correction.
Will I feel the lens in my eye?
You won’t feel phakic lenses after they’re implanted. Unlike external contact lenses that might cause discomfort, these internal implants are “completely unobtrusive after placement”. Your phakic lens “stays in position by itself and does not interact with any of the eye’s structures”.
You might experience minor irritation shortly after surgery, but this comes from the surgical process rather than the lens itself. Take comfort knowing that any discomfort typically resolves within days with proper medication and care.
Is the lens visible to others?
No one will see your phakic lens from the outside. Both main types—posterior chamber and anterior chamber models—remain completely hidden from external view.
Posterior chamber lenses like the Visian ICL sit behind your iris (the colored part of your eye), making them invisible to others. Even anterior chamber lenses like Verisyse, though positioned in front of the iris, aren’t noticeable unless someone examines your eye extremely closely under specialized lighting.
Your vision correction remains your private choice—only your eye doctor will detect the implant during examinations using specialized equipment. This discretion allows you to enjoy improved vision without visible signs of correction.
Conclusion
Phakic lenses have changed the vision correction landscape for patients with severe nearsightedness. Talk with your eye doctor about whether these implants might work for you, especially if you’ve been told LASIK isn’t suitable for your eyes. These remarkable lenses work alongside your natural lens rather than removing or replacing it.
The numbers speak for themselves – clinical studies show 84% of patients achieve 20/40 vision or better with phakic IOLs. For patients with extreme myopia up to -20 diopters, these lenses often deliver better results than any other option available. Your natural focusing ability remains intact, giving you clear vision at different distances.
Like any other procedure in the body, phakic lens implantation carries some risks you should understand. Cataract formation occurs in about 3.7% of cases, while increased eye pressure affects 5-10% of patients. Regular check-ups after surgery help monitor these potential complications and protect your eye health long-term.
Though designed as permanent implants, phakic lenses offer something few other vision corrections can – reversibility. If needed, your doctor can remove these lenses through a simple procedure. This gives many patients peace of mind when considering their options.
Your journey to clear vision starts with understanding all available choices. Book an appointment with an experienced eye surgeon to determine if phakic IOLs might solve your unique vision needs. Through proper evaluation and care, you can make an informed decision about this life-changing procedure.
FAQs
-
What are phakic lenses and how do they work?
Phakic lenses are implantable lenses designed to correct severe nearsightedness. They are surgically placed inside the eye in front of the natural lens, working alongside it to refocus light properly onto the retina and improve vision without removing any eye tissue.
-
Who is an ideal candidate for phakic lens implantation?
Ideal candidates are typically between 21-45 years old with stable vision and high levels of myopia that exceed the safe correction range of laser procedures like LASIK. They should have healthy eyes with sufficient anterior chamber depth and normal endothelial cell counts.
-
What are the main advantages of phakic lenses over other vision correction methods?
Phakic lenses can correct extreme levels of myopia (up to -20 diopters), preserve the eye's natural focusing ability, and offer reversibility if needed. They also avoid risks associated with removing corneal tissue and provide superior visual outcomes for highly myopic eyes compared to laser procedures.
-
What does the recovery process look like after phakic lens surgery?
Most patients return to normal activities within 2-3 days, though complete healing takes about 8 weeks. Vision improvement typically begins within days, with full stabilization in 2-4 weeks. Follow-up visits are crucial, starting just hours after surgery and continuing regularly for several months.
-
What are the potential risks associated with phakic lenses?
While uncommon, risks can include cataract formation, increased intraocular pressure, and gradual loss of corneal endothelial cells. Regular monitoring is essential to detect and manage any complications early. The risk of cataract development is higher in patients over 45 or with very high myopia.