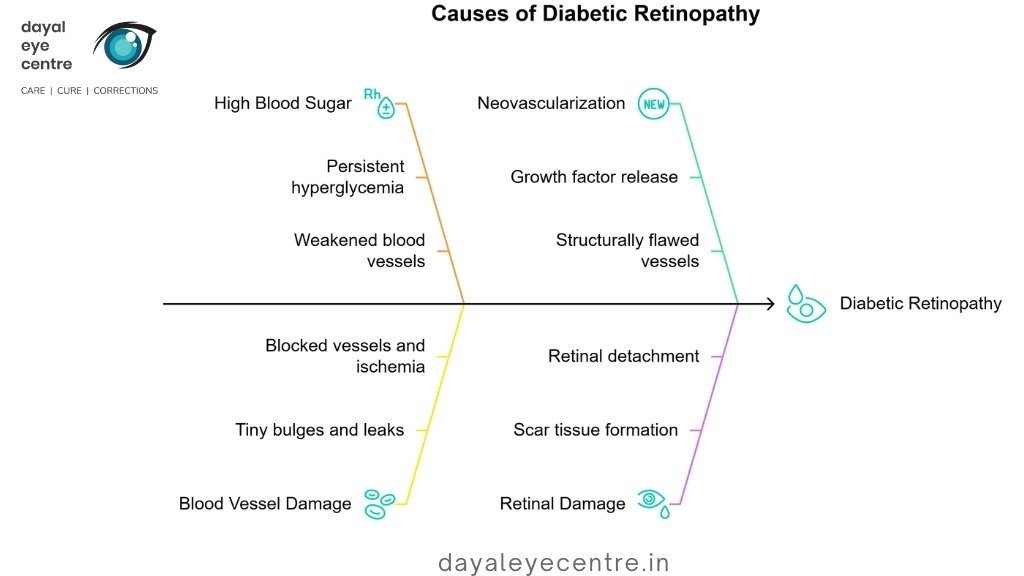
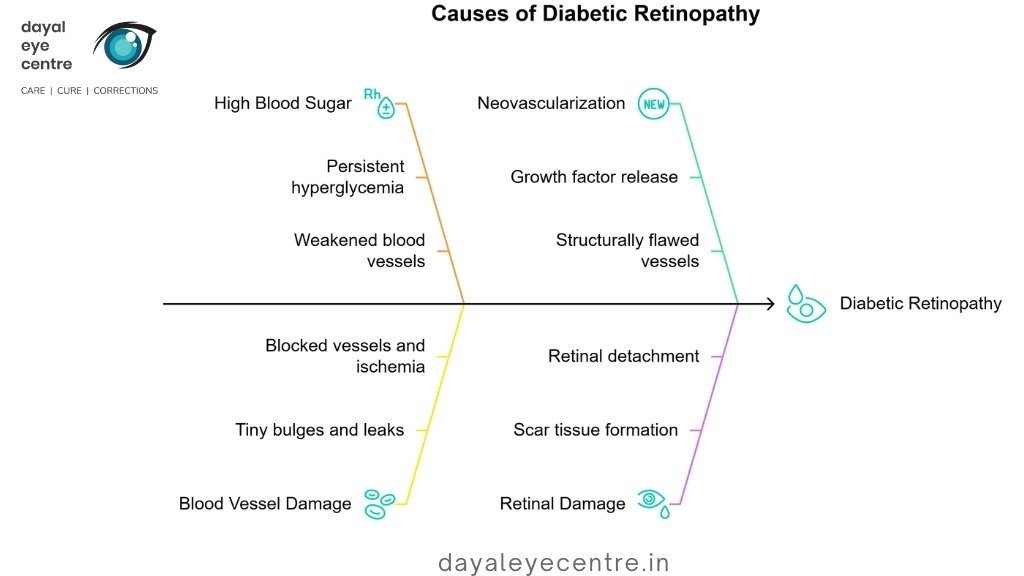
At its core, diabetic retinopathy damages the small blood vessels that nourish your retina. These vessels can undergo several harmful changes – they may swell, leak fluid or blood into the retina, or completely close off, cutting off vital blood supply. Your eye tries to fix this problem by growing new blood vessels, but these new vessels are abnormal and fragile, easily leaking into the clear, jelly-like substance filling your eye (vitreous)…
Doctors classify diabetic retinopathy into two main types:
- Non-proliferative diabetic retinopathy (NPDR) – The early stage where existing blood vessels show damage but no new vessels have formed. During NPDR, tiny bulges (microaneurysms) protrude from vessel walls, sometimes leaking fluid and blood into the retina. This stage progresses from mild to severe as more blood vessels become blocked.
- Proliferative diabetic retinopathy (PDR) – The advanced stage marked by neovascularization (growth of new abnormal blood vessels). These fragile vessels rupture easily, causing vitreous hemorrhage or tractional retinal detachment.
Another important condition that can occur at any stage is diabetic macular edema (DME), which involves swelling of the macula (central portion of the retina) due to fluid buildup. DME represents the most common cause of vision loss in diabetic patients.
Impact of prolonged diabetes on retinal health
The longer you live with diabetes, the higher your risk of developing retinopathy. Over time, more than half of people with diabetes will develop some form of diabetic retinopathy. The primary mechanism of damage involves persistent high blood sugar, which gradually weakens blood vessels throughout your body, particularly the delicate vessels in your retina.
High blood glucose levels trigger a series of harmful changes in your retinal blood vessels. Initially, these vessels develop tiny bulges that can leak fluid. As the condition worsens, more vessels become damaged and blocked, cutting off blood supply to parts of your retina. This creates retinal ischemia (oxygen deprivation), which stimulates the release of growth factors that prompt the formation of new blood vessels.
Unfortunately, these new vessels are structurally flawed and highly permeable. They grow along the retina and into the vitreous gel, where they bleed easily, causing sudden vision loss. The scar tissue that forms can pull on your retina, potentially leading to retinal detachment – a serious complication that causes permanent blindness if not treated promptly.
Eventually, if the damage continues unchecked, it affects the light-detecting cells (photoreceptors) in your retina, causing them to stop functioning properly. Once enough photoreceptors become damaged, permanent vision loss occurs and may progress to blindness.
Who is at Risk and When to Be Concerned
Anyone with diabetes can develop diabetic retinopathy, though certain factors significantly increase your risk. Understanding these factors helps you know when to be concerned and how often to get your eyes examined.
Type 1 vs Type 2 diabetes risk comparison
The relationship between diabetes type and retinopathy shows some surprising patterns. Nearly all Type 1 diabetes patients develop some form of retinopathy after living with the condition for 20 years. In contrast, about 60% of Type 2 diabetes patients show retinopathy symptoms after the same time period.
A key difference appears in when retinopathy first shows up. For Type 1 patients, diabetic retinopathy typically develops later after diagnosis, while Type 2 patients may already have retinopathy when first diagnosed with diabetes. This happens because Type 2 diabetes often remains undetected for years before diagnosis.
Despite developing later, research suggests Type 2 diabetes might actually pose a greater threat to vision. After 15 years with diabetes, 52.7% of those with Type 2 diabetes developed retinopathy compared to 30.6% of those with Type 1. People with youth-onset Type 2 diabetes had an 88% higher risk for any form of diabetic retinopathy compared to those with Type 1.
The duration of diabetes remains the strongest predictor for retinopathy development regardless of type. For younger patients, the numbers tell a concerning story: 8% at 3 years, 25% at 5 years, 60% at 10 years, and 80% at 15 years.
Pregnancy-related diabetic eye disease
Pregnancy creates a unique risk environment for diabetic retinopathy. Women with diabetes who become pregnant face a substantially higher risk of developing or worsening retinopathy compared to non-pregnant diabetic individuals.
The prevalence of diabetic retinopathy in early pregnancy varies significantly by diabetes type:
- Type 1 diabetes: 34-72% of pregnant women
- Type 2 diabetes: 14% of pregnant women
- Gestational diabetes: 10-27% of women
Several factors influence retinopathy progression during pregnancy. Surprisingly, rapid improvement in blood glucose control during pregnancy paradoxically increases retinopathy risk. This occurs because sudden normalization of blood sugar can temporarily worsen retinal damage.
Pregnancy-induced hypertension considerably escalates retinopathy risk, with studies showing progression in 50% of women with pregnancy-induced hypertension compared to 25% in those without hypertension. Furthermore, women with preexisting retinopathy before conception face significantly higher risks of further deterioration.
Influence of hypertension and cholesterol
Beyond diabetes itself, certain other health conditions substantially increase retinopathy risk. Like any other procedure in the body, your eyes respond to your overall health status.
Hypertension emerges as a major contributor to diabetic retinopathy development and progression. Studies show that hypertensive diabetic patients have more than twice the risk of developing retinopathy compared to those with controlled blood pressure. This happens because hypertension compounds vascular damage, further injuring the already compromised retinal blood vessels.
Likewise, lipid abnormalities directly impact retinopathy risk. Research links high cholesterol with specific retinopathy complications, especially hard exudates and macular edema. Higher levels of total cholesterol, LDL-C, and triglycerides serve as warning signs for developing hard exudates in diabetic patients.
Besides these major factors, other risk elements include:
- Ethnic background (higher risk for Black, Hispanic, and Native American populations)
- Tobacco use
- Kidney disease (especially in early stages for Type 1 diabetes)
- Late introduction of insulin therapy in Type 2 diabetes
Talk with your eye doctor about your personal risk factors. Regular comprehensive eye examinations remain crucial, specifically tailored to your individual risk profile. Even without symptoms, early detection through screening provides the best opportunity to preserve your vision.
How Diabetic Retinopathy Progresses Over Time
Your eyes change in predictable ways as diabetic retinopathy develops. Understanding these stages helps you and your doctor monitor your eye health and catch problems early. Like any other procedure in the body, your retina responds to high blood sugar with a series of changes that follow a specific pattern.
Background retinopathy and early vessel changes
Background retinopathy marks the first stage of this condition. Tiny swellings called microaneurysms in the retina’s blood vessels appear like small bulges on a garden hose. These weak spots can leak small amounts of blood and fluid into your retina.
The concerning part? You typically won’t notice any vision changes at this early stage despite the damage already occurring. Your eyes don’t send warning signals – the walls of your blood vessels silently weaken, and capillaries become increasingly fragile. Regular eye screening becomes essential since these early changes usually only show up during a professional eye exam.
Pre-proliferative stage and ischemic damage
As your condition advances to pre-proliferative retinopathy, more serious and widespread changes appear in your retinal blood vessels. Think of it as a river system experiencing multiple blockages – your blood vessels swell further, blocking blood flow and preventing proper nourishment to retinal tissues.
This stage includes several distinctive features:
- Intraretinal microvascular abnormalities (IRMAs)
- Venous beading and irregularities
- Cotton wool spots indicating nerve fiber damage
- More significant retinal hemorrhages
The blockage of blood vessels creates areas of retinal ischemia (oxygen deprivation), triggering the release of growth “factors” including vascular endothelial growth factor (VEGF). Your risk of eventual vision problems increases substantially at this stage.
Proliferative stage with neovascularization
Proliferative diabetic retinopathy represents the most advanced and dangerous stage. The hallmark feature is neovascularization—your eye attempts to solve its oxygen problem by growing new blood vessels. Unfortunately, these new vessels are remarkably fragile, thin-walled, and prone to bleeding.
The abnormal vessels grow along the surface of your retina and into the vitreous gel. Over time, they form scar tissue that can contract and pull on your retina, potentially causing tractional retinal detachment. This detachment results in blurriness, reduced field of vision, and even permanent blindness if left untreated.
Approximately 7% of people with diabetes develop proliferative retinopathy, with numbers increasing with disease duration, particularly in Type 1 diabetes. Without appropriate treatment, this stage presents a very high risk of irreversible vision loss.
Talk with your eye doctor about your specific risk factors and how often you should have your eyes examined. Early detection gives you the best chance of preserving your vision.
Complications Arising from Untreated Retinopathy
Untreated diabetic retinopathy leads to serious complications that can permanently damage your vision. Like any other procedure in the body, your eyes need proper care to prevent these advanced problems. Without treatment, this progressive eye disease develops into several serious conditions that need immediate medical attention.
Diabetic Macular Edema and Central Vision Loss
Diabetic macular edema (DME) happens when fluid leaks into your macula—the central part of your retina responsible for sharp, detailed vision. This leakage causes your macula to swell, distorting what you see directly in front of you. For many patients, DME creates blurry or wavy images, especially when looking straight ahead. Objects might appear different sizes when viewed with each eye separately, and colors often look dull or faded.DME affects approximately 1 in 15 people with diabetes and represents the most common reason diabetic patients lose their vision.
The severity of vision loss typically depends on how much fluid builds up and how long it remains. The window for saving your sight gets smaller the longer DME goes untreated. Studies show that Black and Hispanic/Latinx individuals face higher rates of serious vision loss from DME.
Tractional Retinal Detachment
In advanced stages of diabetic retinopathy, abnormal blood vessels stimulate scar tissue growth that can pull your retina away from the back of your eye. This tractional retinal detachment (TRD) occurs in about 5% of people with proliferative diabetic retinopathy. The contractile forces of these fibrous membranes create a concave retinal configuration between elevated areas.
You might notice TRD symptoms like floating spots, flashes of light, or severe vision loss. Chronic macular detachments often lead to permanent damage to your light-detecting cells, preventing useful vision from returning. Without treatment, even minor retinal detachment can progress to blindness.
Neovascular Glaucoma and Optic Nerve Damage
Neovascular glaucoma (NVG) develops when abnormal blood vessels grow into the front part of your eye, blocking fluid drainage and causing dangerous pressure increases. This elevated pressure damages your optic nerve, causing vision loss that can progress to blindness.
Proliferative diabetic retinopathy stands as the leading cause of NVG. The reported prevalence of NVG is 2.1% in all diabetic patients but rises dramatically to 21.3% in those with proliferative diabetic retinopathy. NVG represents a terminal diabetic complication with significant connections to diabetic neuropathy and kidney disease.
The medical management of these complications often requires aggressive treatment with high failure rates—up to 62.8% for NVG. Regular check-ups with your eye doctor help monitor healing and address concerns promptly. If you experience severe pain or worsening symptoms, seek immediate medical attention.
Talk with your eye doctor about how often you should have your eyes examined based on your risk factors. Early detection and treatment remain your best defense for preserving vision.
Managing and Treating Diabetic Retinopathy Effectively
Effective management of diabetic retinopathy starts long before your vision shows problems. With the right approach for each stage, you can greatly reduce your risk of vision loss.
Importance of A1C Control and Lifestyle Changes
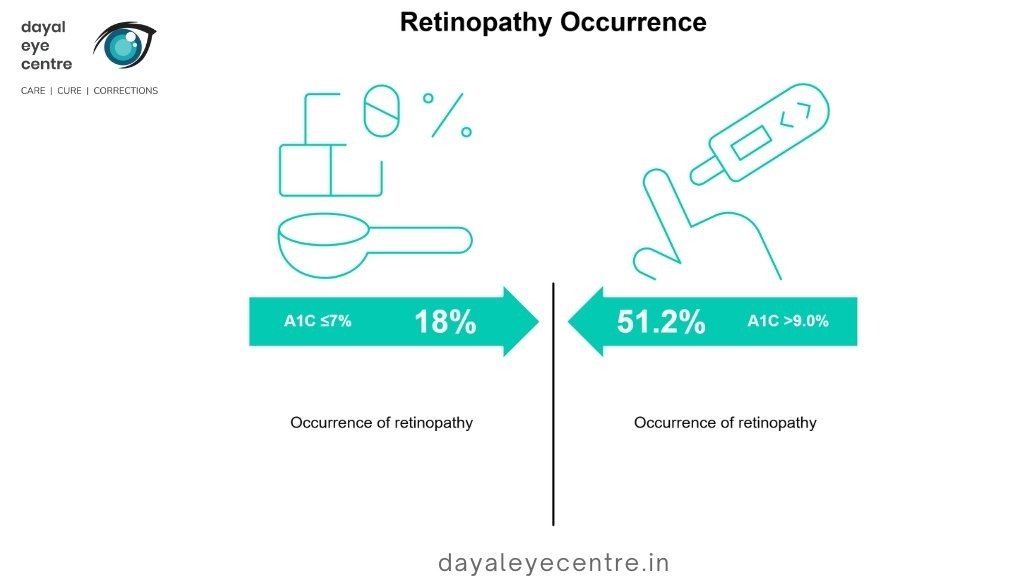
Blood sugar management forms the foundation of preventing and treating diabetic retinopathy. Research clearly links higher A1C levels with increased retinopathy risk. Your doctor will likely recommend aiming for an A1C below 7%, as each 1% increase raises your risk of retinopathy progression by 15.4%.
Even small improvements make a real difference—studies show retinopathy appears in only 18% of patients with A1C ≤7% compared to 51.2% in those with A1C >9.0%.
Beyond glucose control, managing blood pressure (aiming for <130/80 mm Hg) and cholesterol simultaneously helps protect your retinal vessels. To support your eye health:
- Follow a low-sugar, high-fiber diet with whole grains and vegetables
- Get at least 150 minutes weekly of moderate physical activity
- Maintain consistent eating patterns to keep blood glucose stable
The way the way smudgy lenses cause blurry vision, poorly controlled diabetes can similarly damage your sight. Talk with your doctor about creating a management plan that works for your lifestyle.
While tight glucose control provides long-term benefits, a sudden drop in A1C can temporarily worsen retinopathy. This “early worsening” happens in (10-20%) of patients after rapid blood sugar improvement. Your doctor can help manage this transition safely.
Medical Treatments: Injections, Laser, Surgery
For active retinopathy, several treatments prove effective:
Intravitreal injections deliver medication directly into your eye’s vitreous. Anti-VEGF drugs like ranibizumab (Lucentis) and aflibercept (Eylea) stop abnormal vessel growth and reduce fluid leakage. Steroid injections or implants help control inflammation and swelling. Most patients need need injections for typically six months or more, depending on response.
Laser treatments work in two main ways: focal laser targets specific leaking vessels in diabetic macular edema, while scatter (panretinal) photocoagulation shrinks abnormal vessels in proliferative retinopathy. You’ll typically need between 1-3 laser sessions.
Vitrectomy surgery becomes necessary when proliferative retinopathy causes significant bleeding or retinal detachment. This procedure removes blood from the vitreous and relieves pulling on the retina, with success rates around 90%.
The good news? These treatments have transformed diabetic retinopathy care, helping preserve vision that would have been lost just decades ago.
Monitoring Frequency Based on Disease Stage
Like any other procedure in the body, diabetic retinopathy requires regular check-ups. How often you need eye exams depends on your condition:
- No retinopathy: Every 1-2 years
- Mild/moderate non-proliferative: Every 6-8 months
- Severe non-proliferative: Every 3-4 months
- Proliferative or macular edema: Every 2-3 months
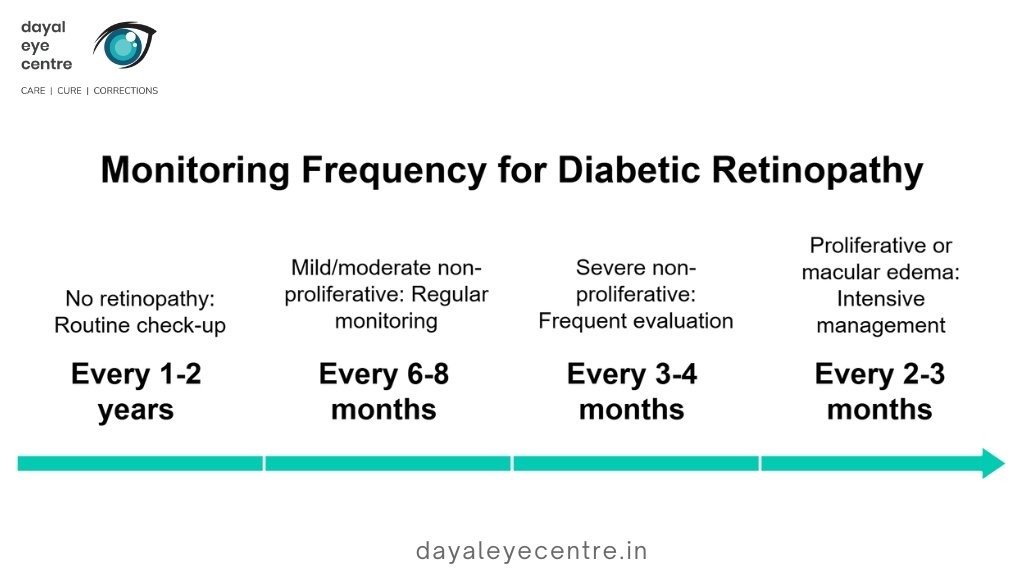
Pregnant women need closer monitoring, with eye exams recommended before conception or during the first trimester. This approach catches problems early while avoiding unnecessary visits—proper scheduling may reduce the number of retinal exams over a patient’s lifetime by up to 58% while still detecting advanced disease promptly.
Your eye doctor will help create a monitoring schedule that matches your specific situation. Regular visits help catch changes early when treatment works best.
Conclusion
Diabetic retinopathy stands as one of the biggest threats to vision for people living with diabetes. Throughout this article, you’ve learned how this condition develops, moves through different stages, and can eventually threaten your sight if left untreated. Many patients don’t know they have retinopathy until symptoms become obvious – a concerning fact since early treatment significantly improves outcomes.
The numbers tell a clear story: maintaining tight blood sugar control is your first line of defense against retinopathy development and progression. Your vision stability depends on managing blood pressure and cholesterol levels as well. Regular eye screening based on your personal risk – whether yearly for those without retinopathy or every few months for advanced cases – helps catch changes before permanent damage occurs.
Medical treatments have improved dramatically in recent years. Anti-VEGF injections, laser procedures, and vitrectomy surgery now offer effective options at different disease stages. The good news? These treatments work best when started early, before significant damage accumulates.
Like any other procedure in the body, retinopathy management requires a complete approach. Blood sugar control remains essential, though lifestyle changes and proper medical care together create the strongest protection against vision loss. Talk with your eye doctor about creating a monitoring plan tailored to your specific situation.
The journey with diabetes presents many challenges, yet with careful eye care and proper disease management, you can effectively preserve your vision for years to come. Through regular check-ups and following your doctor’s recommendations, most patients maintain good vision despite their diabetes diagnosis.
FAQs
What causes diabetic retinopathy?
Diabetic retinopathy is primarily caused by prolonged high blood sugar levels associated with diabetes. Over time, elevated glucose damages the tiny blood vessels in the retina, leading to various eye complications.
How can diabetic retinopathy be effectively managed?
Effective management includes maintaining tight blood sugar control (generally aiming for an A1C below 7%), regular eye screenings, and lifestyle modifications such as a healthy diet and regular exercise. Medical treatments like anti-VEGF injections, laser therapy, or surgery may be necessary in advanced cases.
Is it possible to prevent diabetic retinopathy from progressing?
While diabetic retinopathy cannot always be prevented, its progression can often be slowed or halted through proper diabetes management, regular eye exams, and timely treatment. However, ongoing monitoring is crucial as the risk of future retinal damage remains.
What are the main stages of diabetic retinopathy
Diabetic retinopathy progresses through several stages: background retinopathy (early vessel changes), pre-proliferative retinopathy (more severe vessel damage), and proliferative retinopathy (growth of abnormal new blood vessels). Each stage requires different management approaches.
Who is at highest risk for developing diabetic retinopathy?
While all individuals with diabetes are at risk, those with longer diabetes duration, poor blood sugar control, high blood pressure, or high cholesterol face increased risk. Pregnant women with diabetes and certain ethnic groups (such as Black, Hispanic, and Native American populations) also have higher risk profiles.