A retinal vein occlusion disrupts your eye’s delicate circulatory system. Interruption of blood flow in these vital visual structures makes it essential to understand how this condition works. Both patients and clinicians need this knowledge to manage the condition effectively.
How blood flow is disrupted in the retina
Your retina has a network of arteries that supply oxygen-rich blood and veins that carry blood away. Retinal vein occlusion (RVO) occurs when a vein becomes partially or completely blocked. This blockage usually results from the formation of a thrombus (blood clot). The condition develops through Virchow’s triad of thrombogenesis: venous stasis, degenerative changes in vessel walls, and blood hypercoagulability.
Arterial stiffness plays a decisive role in many cases. Atherosclerosis causes arteries to harden, leading them to compress nearby veins. This compression occurs especially at arteriovenous crossings, where both vessels share a common connective tissue sheath. Blood flow becomes turbulent, promoting clot formation. The blocked vessels cause pressure to build in the capillaries, leading to blood and fluid leakage into the surrounding retinal tissue.
Branch retinal vein occlusions (BRVO) typically develop at these arteriovenous intersections. Central retinal vein occlusion (CRVO) usually occurs at the lamina cribrosa, where the central retinal vein exits the eye
Macular edema and neovascular complications
Blocked blood flow creates localized hypoxia (oxygen deprivation), which triggers the release of vascular endothelial growth factor (VEGF). This protein leads to two main complications:
First, VEGF increases vascular permeability, resulting in macular edema. This condition occurs when fluid accumulates in the macula—the central part of the retina responsible for sharp, central vision. Vision loss in patients with RVO primarily occurs due to this swelling.
Second, persistent oxygen deprivation stimulates abnormal new blood vessel growth (neovascularization). These new vessels are fragile and prone to leakage, leading to several complications depending on their location, including:
- Vitreous hemorrhage (bleeding into the eye’s gel-like interior)
- Retinal detachment
- Neovascular glaucoma (when new vessels form in the iris or drainage angle)
Research shows that 52% of patients with ischemic CRVO develop iris neovascularization, and about 34% develop neovascular glaucoma within nine months. Early treatment is therefore vital, even in non-ischemic cases.

Differences between CRVO and BRVO
The location of the blockage determines whether a patient has CRVO or BRVO. Each type has distinct mechanisms, severity levels, and outcomes.
CRVO affects the central retinal vein at or behind the lamina cribrosa, causing hemorrhages across all four retinal quadrants. Patients usually experience more severe vision loss with CRVO than with BRVO. Clinicians classify CRVO into ischemic (non-perfused) and non-ischemic (perfused) types. The ischemic form accounts for about 30% of cases and is associated with poorer outcomes. Approximately 80% of these patients maintain visual acuity worse than 20/200.
BRVO affects only one branch of the retinal venous system. Most cases occur in the superotemporal quadrant (58–66%). Patients generally have better outcomes with BRVO than with CRVO. Studies show that 40% of untreated BRVO eyes improved after three years, and about 80% of cases demonstrated improved or stable vision over time.
The risk of complications varies significantly between the two types. Non-ischemic CRVO can convert to the ischemic form—15% within the first four months and 34% after three years. Patients with ischemic CRVO face a higher risk of neovascular glaucoma. This condition is often referred to as “90-day glaucoma” because it can develop rapidly.
Recognizing the Symptoms of RVO
Early detection of retinal vein occlusion (RVO) can affect treatment outcomes by a lot. Symptoms vary among patients, so knowing what to look for is vital for anyone at risk.
Sudden or gradual vision loss
Vision loss is the primary symptom of retinal vein occlusion. It may occur suddenly or develop gradually over time. This change in vision is usually painless and typically affects only one eye.
Patients with central retinal vein occlusion (CRVO) often experience sudden vision loss that may involve the entire visual field. Some notice a dense central scotoma (blind spot) that develops quickly, while others experience subtle or intermittent episodes of blurred vision. The severity of symptoms depends on whether the CRVO is ischemic or non-ischemic, with ischemic cases usually producing more severe symptoms.
Branch retinal vein occlusion (BRVO) typically presents as partial vision loss in the area supplied by the blocked vessel. Many cases are asymptomatic, particularly when the affected area is not near the macula. Such cases are often detected during routine eye examinations.
Vision changes can range from mild blurring to significant vision loss. Although RVO rarely causes complete blindness, visual quality often does not return to normal, even with treatment.
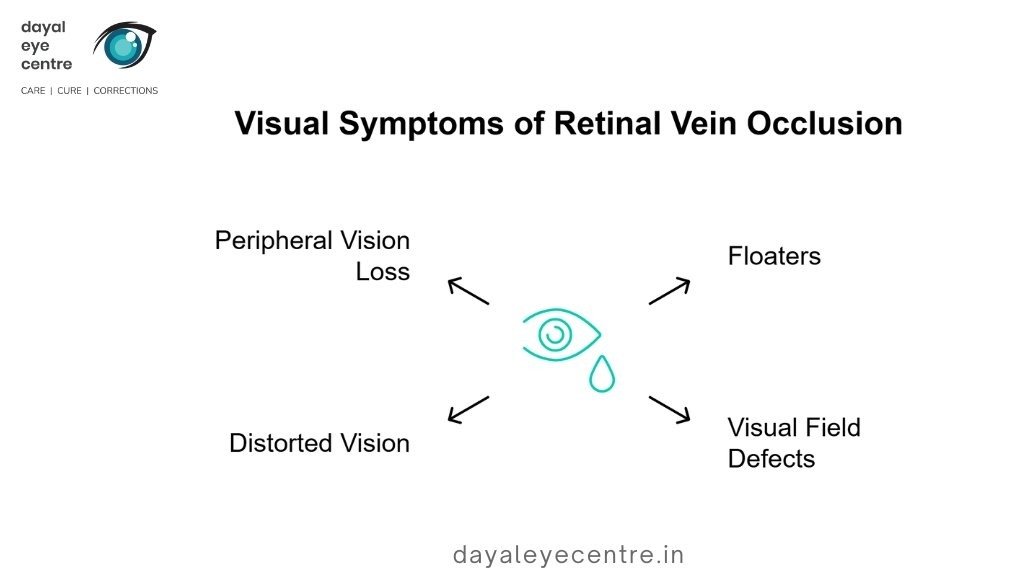
Presence of floaters and visual field gaps
RVO can cause several visual disturbances, including:
- Floaters: Dark spots, lines, or squiggly shapes in the vision. Floaters associated with RVO may indicate vitreous hemorrhage due to neovascularization (abnormal blood vessel growth).
- Visual field defects: Areas of partial vision loss or blind spots in specific regions of the visual field.
- Distorted vision: Objects may appear warped or wavy, especially if macular edema develops.
- Peripheral vision loss: Side vision may decline, particularly in severe cases.
These symptoms occur when fluid and blood leak into the retina due to increased pressure behind the blockage. The macula, which is responsible for detailed central vision, often swells with excess fluid, leading to blurring.
When to seek emergency care
Quick action can save your vision. You should seek emergency care if you notice:
- Sudden vision loss in one eye – This requires urgent evaluation. Although some sources suggest sudden vision loss is not typical of RVO, multiple reliable sources confirm that it can occur, especially with CRVO.
- Significant vision decrease over hours or days – Rapid vision loss needs immediate attention.
- New floaters with vision changes – This is especially important if you also notice visual field defects.
Subtle blurring or minor visual changes may wait a few days until you see an ophthalmologist. However, all vision changes should be evaluated, as early treatment reduces the risk of permanent vision loss.
Eye pressure or pain may occur in severe CRVO cases that develop neovascular glaucoma. Any eye pain associated with vision changes requires immediate medical attention.
It is also important to note that non-ischemic CRVO can progress to the more dangerous ischemic form over time. This makes proper evaluation of all visual symptoms essential, regardless of their initial severity.
What Causes Retinal Vein Occlusion to Develop
Understanding the mechanisms of retinal vein occlusion helps clinicians identify high-risk patients and develop prevention strategies. Multiple factors often work together to create conditions that lead to venous blockage.
Role of high blood pressure and cholesterol
High blood pressure is the most significant risk factor for retinal vein occlusion. Persistently elevated blood pressure leads to atherosclerosis, causing blood vessels to become stiff and narrow. These hardened arteries compress nearby veins, particularly at arteriovenous crossing points where arteries and veins share connective tissue. The compressed veins create turbulent blood flow, damaging the vessel lining and promoting clot formation.
Research clearly supports this association. Studies show that high blood pressure significantly increases RVO risk, with hazard ratios of 1.10 for elevated blood pressure, 1.07 for stage 1 hypertension, and 1.32 for stage 2 hypertension. Effective blood pressure control reduces RVO risk by 27% in patients with stage 2 hypertension.
High cholesterol levels also contribute to RVO development. Studies demonstrate higher rates of hyperlipidemia in both central and branch retinal vein occlusion patients (p < 0.001). Low HDL cholesterol is associated with an increased risk of RVO (hazard ratio 1.12).
Impact of diabetes and glaucoma
Diabetes contributes to RVO through several mechanisms. Elevated blood glucose damages small blood vessels, causing arteriolar rigidity and narrowing of retinal vessels. Additionally, diabetes accelerates arteriosclerosis, increasing the risk of thromboembolism, the primary cause of RVO.
Glaucoma and RVO have a complex relationship. Elevated intraocular pressure can displace the lamina cribrosa, altering the shape of the central retinal vein and increasing blood flow turbulence. People with diabetes have twice the risk of developing glaucoma compared to the general population. Glaucoma occurs twice as often in hemi-retinal vein occlusion (HRVO) as in CRVO and four times more often than in BRVO.
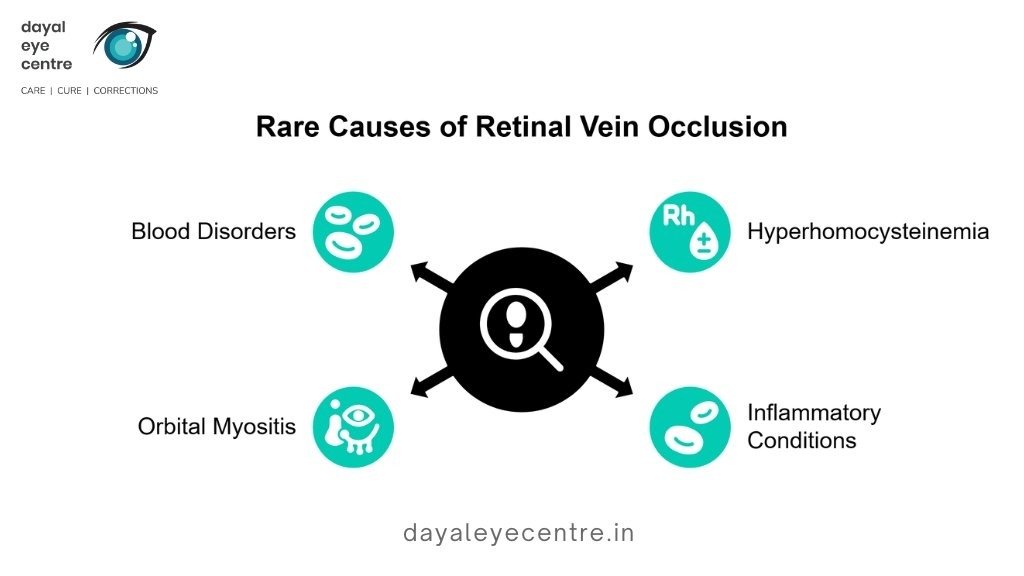
Blood clotting disorders and rare causes
Blood clotting disorders are more commonly implicated in younger patients with RVO, while cardiovascular conditions are more frequent contributors in older patients. Individuals under 45 with RVO show higher rates of activated protein C resistance (p = 0.014), antiphospholipid antibodies (p = 0.022), and anticoagulant protein deficiencies (p = 0.05).
Several rare conditions can also lead to RVO, including:
- Hyperhomocysteinemia
- Inflammatory conditions such as vasculitis
- Orbital myositis and other orbital inflammatory diseases
- Blood disorders, including polycythemia vera
Retinal artery occlusion vs vein occlusion
Retinal artery occlusions differ from vein occlusions, although they may appear similar. Retinal artery occlusion (RAO) is usually caused by emboli rather than local blood clots, making it a true “eye stroke” that requires immediate medical attention. RAO is less common than retinal vein occlusion (RVO) but typically results in more severe vision loss.
Both conditions share risk factors such as high blood pressure, diabetes, and atherosclerosis. However, RAO has a stronger association with cardiac emboli, particularly in patients with atrial fibrillation. Patients with RAO require urgent evaluation for stroke risk, while those with RVO typically undergo assessment for underlying vascular disorders.
How doctors diagnose RVO and assess damage
Accurate diagnosis is essential for effective management of retinal vein occlusion (RVO). Eye care specialists use several diagnostic tools to confirm the condition and assess the extent of retinal damage.
Eye dilation and retinal examination
Diagnosis begins with a dilated fundus examination. Eye drops are used to widen the pupils, allowing detailed visualization of the retina. Central retinal vein occlusion (CRVO) often shows a characteristic “blood and thunder” appearance, with widespread hemorrhages across all quadrants, cotton wool spots, and optic disc swelling. Non-ischemic CRVO presents with mild venous dilation and fewer hemorrhages, while ischemic CRVO shows marked retinal edema and extensive hemorrhaging. Branch retinal vein occlusion (BRVO) typically presents with hemorrhages and edema confined to the affected retinal sector.
OCT and OCTA imaging for macular thickness
Optical coherence tomography (OCT) is a cornerstone of RVO evaluation. This non-invasive imaging technique provides high-resolution cross-sectional images of the retina, allowing precise measurement of macular thickness and detection of fluid accumulation. Treatment decisions are often guided by OCT findings. Optical coherence tomography angiography (OCTA), an advanced form of OCT, visualizes retinal blood vessels without the use of dye and helps assess vessel density and changes in the foveal avascular zone, aiding differentiation between ischemic and non-ischemic RVO.
Fluorescein angiography for vessel leakage
Fluorescein angiography involves injecting a dye into a vein in the arm, which then circulates through the retinal blood vessels and becomes visible during imaging. This test identifies delayed venous filling, capillary nonperfusion, vascular leakage, and neovascularization. These findings help retinal specialists assess the severity of ischemia and plan appropriate treatment.
Visual acuity and field tests
Visual acuity testing using standardized charts after refraction is part of functional vision assessment. Visual field testing detects scotomas (blind spots) and peripheral vision defects. These tests establish baseline vision and help monitor response to treatment. Additional evaluations may include pupillary response testing, intraocular pressure measurement, and blood tests to identify underlying systemic conditions, particularly in younger patients or those with atypical presentations.
Available Treatments and Long-Term Management
Doctors can’t directly unblock occluded veins in retinal vein occlusion, so they focus on treating complications. Treatment plans change based on how severe the condition is and what complications arise.
Anti-VEGF therapy and bispecific antibodies
Because occluded retinal veins cannot be directly reopened, treatment focuses on managing complications. Management strategies vary depending on disease severity and associated complications.
Anti-VEGF therapy and bispecific antibodies
Anti-VEGF injections are the first-line treatment for macular edema secondary to RVO. These medications reduce VEGF levels, decreasing retinal swelling and improving vision. Commonly used agents include:
- Bevacizumab (Avastin): Effective despite off-label use
- Ranibizumab (Lucentis): FDA-approved, with studies showing a 16–18 letter improvement in visual acuity compared to 7.3 letters in control groups
- Aflibercept (Eylea): Demonstrates an average improvement of 17.7 letters at 24 weeks compared with −0.5 letters in sham-treated patients
Treatment usually requires repeated injections over months or years, initially administered every one to two months. Faricimab (Vabysmo), a newer bispecific antibody, targets both VEGF-A and angiopoietin-2 pathways. Clinical trials have shown that nearly 60% of BRVO patients and 48% of CRVO patients were able to extend treatment intervals to three to four months.
Steroid injections and their limitations
Steroid therapy may be considered when anti-VEGF treatment is insufficient. The dexamethasone intravitreal implant (Ozurdex) typically shows peak effectiveness about two months after administration, with patients gaining an average of 10 letters in visual acuity. Intravitreal triamcinolone acetonide is another option, with a 4 mg dose lasting one to four months and higher doses lasting up to nine months.
Despite their effectiveness, steroids carry notable risks. Approximately 35% of patients receiving 4 mg triamcinolone require medication to control elevated intraocular pressure, compared with 8% in observation groups. Steroid treatment also increases the risk of cataract formation, occurring in about 33% of treated patients versus 18% in untreated patients.
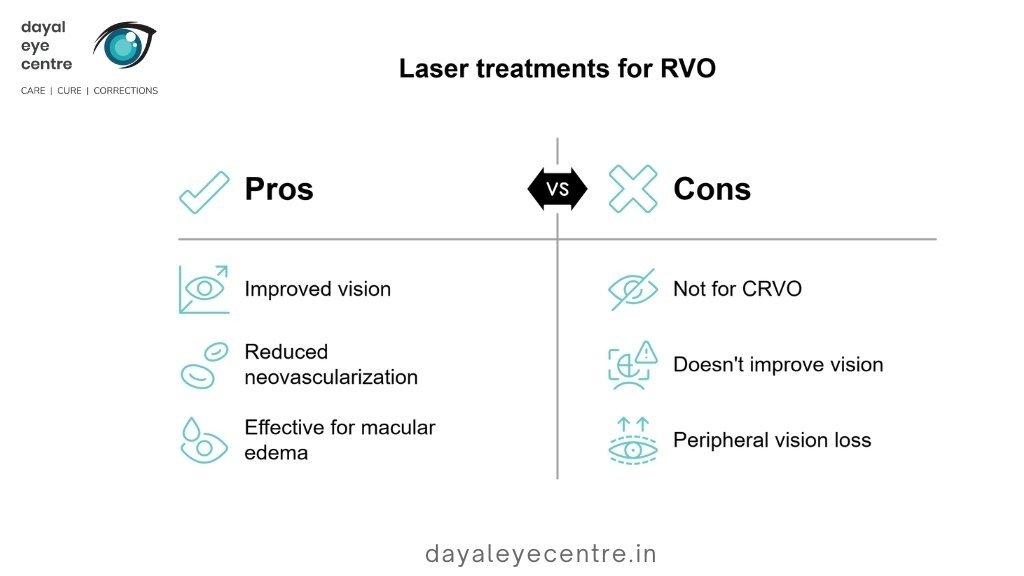
Laser photocoagulation and PRP
Laser therapy is used for specific RVO-related complications. Grid laser photocoagulation is primarily used for macular edema associated with BRVO rather than CRVO. The Branch Vein Occlusion Study demonstrated improved visual outcomes with grid laser treatment compared with observation alone.
Panretinal photocoagulation (PRP) is used to manage neovascularization. By creating controlled burns in the peripheral retina, PRP reduces VEGF production and lowers the risk of further neovascular complications. Although PRP does not directly improve vision, it significantly reduces the likelihood of vision-threatening sequelae.
Vitrectomy for severe complications
Surgery is required when patients develop persistent vitreous hemorrhage, recurrent bleeding lasting more than four weeks, or retinal detachment. During a vitrectomy, the surgeon removes the vitreous gel and repairs retinal damage. Laser treatment may also be applied, and the vitreous is replaced with saline, gas, or silicone oil. Research indicates that carefully selected patients can achieve better long-term visual outcomes after vitrectomy.
Lifestyle changes and risk factor control
Preventing recurrence of RVO depends largely on managing underlying conditions. The risk can be reduced by controlling high blood pressure, diabetes, and cholesterol levels. Regular follow-up visits, particularly during the first few months, help clinicians detect and manage complications early. Adopting a healthy lifestyle—including regular exercise, smoking cessation, and maintaining a healthy weight—supports long-term disease management.
Conclusion
Retinal vein occlusion poses a serious threat to vision if not treated promptly. This article has explained how disruption of retinal blood flow leads to complications such as macular edema and neovascularization, both of which can cause permanent vision loss. Although patients with BRVO generally have better outcomes than those with CRVO, both conditions require timely medical attention.
Early recognition of symptoms plays a crucial role in outcomes. Sudden vision changes, new floaters, or visual field defects should prompt immediate evaluation. Eye care specialists rely on advanced diagnostic tools such as OCT imaging, fluorescein angiography, and comprehensive eye examinations to assess retinal damage and formulate appropriate treatment plans.
Although there is currently no method to directly reopen an occluded retinal vein, modern treatments effectively manage complications. Anti-VEGF injections, including newer bispecific antibodies such as faricimab, have significantly improved visual outcomes for many patients. Steroid therapies serve as alternative options, despite their potential side effects. Laser procedures and vitrectomy surgery are valuable for managing severe or vision-threatening complications.
Medical treatment is most effective when combined with good systemic health management. Patients should work closely with their healthcare providers to control blood pressure, manage diabetes, and maintain healthy cholesterol levels. Regular eye examinations enable early detection of changes that require intervention.
Advances in modern ophthalmology offer hope for preserving vision. Prompt attention to visual symptoms is essential. With appropriate treatment and long-term commitment to care, many patients with RVO can maintain functional vision and lead fulfilling lives.
FAQs
What are the most effective treatments for retinal vein occlusion?
Primary treatments include anti-VEGF injections to reduce macular edema, steroid injections, laser photocoagulation for selected complications, and vitrectomy surgery in severe cases. Management also involves controlling underlying risk factors such as hypertension and diabetes.
What are the main risk factors for developing retinal vein occlusion?
Key risk factors include high blood pressure, high cholesterol, diabetes, and glaucoma. Increasing age, particularly over 50 years, also raises risk. Blood clotting disorders may contribute, especially in younger patients.
How quickly should I seek medical attention if I experience sudden vision changes?
Immediate medical care is required for sudden vision loss, rapid vision decline over hours or days, or new floaters accompanied by vision changes. Even mild or subtle symptoms should be evaluated by an ophthalmologist within a few days.
Can retinal vein occlusion resolve on its own without treatment?
Some mild cases may show partial improvement without treatment, but most cases- especially severe forms—do not recover on their own and may worsen. Early treatment is critical to preserve vision.
How do doctors diagnose retinal vein occlusion?
Diagnosis typically includes a dilated eye examination, optical coherence tomography (OCT) to assess macular thickness, fluorescein angiography to evaluate vascular leakage, and visual acuity and visual field testing. These tests confirm RVO and help determine the extent of retinal damage.