Tractional: This happens when scar tissue on the retina pulls it away from the back of the eye. This type of retinal detachment is common among those with diabetes. If you have prolonged high blood sugar levels, it can damage the blood vessels in your eye, leading to scar tissue formation in the back of your eye. As the scars and areas of traction keep getting bigger, it increases the chances of it pulling and detaching the retina from the back of the eye.
Exudative: In this scenario, fluids build up behind the retina even though there’s no retinal tear. As the fluids keep collecting behind the retina, it eventually pushes your retina away. The main causes of this fluid buildup are leaking blood vessels or swelling behind the eye, which can happen from such causes as uveitis or an eye injury or conditions that cause swelling or leaking blood vessels.
Besides retina detachment showing early symptoms, certain factors increase the chances of it occurring. They mainly include the following conditions,
The most common methods of diagnosing retinal detachment include
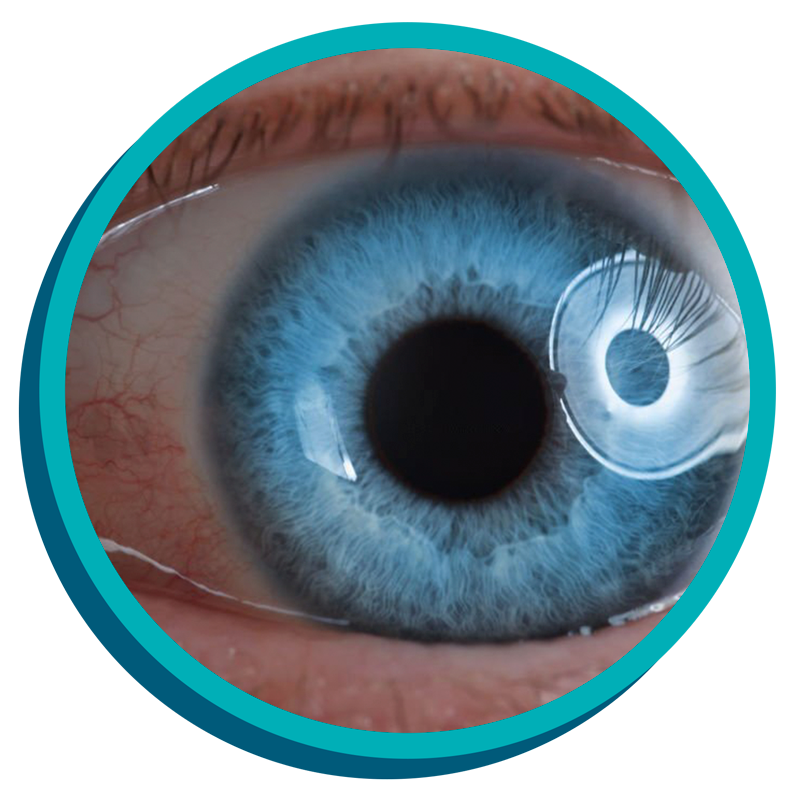
Optical Coherence Tomography: In the most common and simple method of diagnosis, your ophthalmologist will put drops in your eye to dilate and widen the pupil. Then, they will look through a special lens to check your retina for any damages or changes or damages, this is known as optical coherence tomography (OCT).
Treatment for retinal detachment usually involves surgery, and the types of procedures usually involved are as follows.
Pneumatic Retinopexy: At the beginning of this procedure, your ophthalmologist will put a gas bubble inside your eye. This will push the retina into place so it can heal properly. Afterwards, your doctor will instruct you to keep your head in a very specific position for a few days. This position will keep the bubble in the right place. As your eye heals over time, your body makes fluid that fills the eye and this fluid will replace the gas bubble.
Vitrectomy: This procedure is done to remove the vitreous fluid that’s pulling on the retina. The vitreous fluid will be replaced with an air, gas, or oil bubble. The bubble will push the retina into place so it can heal properly. If an oil bubble is used, then it will be removed a few months later. If an air or gas bubble is used, you will not be allowed to fly in an aeroplane, travel to high altitudes, or scuba dive. This is because the change in altitude will cause the gas bubble to expand, thus increasing eye pressure.
Scleral Buckle: In this procedure, a band of rubber or soft plastic is sewn to the outside of your eyeball. It will help in gently pressing your eye inward, thus causing the detached retina to heal against the eye wall. The scleral buckle cannot be seen in the eye and it is usually left on the eye permanently.
As many risks and factors contribute to retina detachment, it helps to know some precautionary measures that you can take beforehand. This will usually include,
Dayal eye centre
808 B, Galaxy Road, Sector 15 Part 2,
Near 32nd Avenue, Gurgaon, Haryana 122001
wecare@dayaleyecentre.in