Recognizing early symptoms of retinal detachment can save your vision. These warning signs occur because the retina—the light-sensitive layer at the back of the eye—begins to pull away from its normal position. Like other parts of the body, the retina sends clear signals when something is wrong.
Seeing new floaters suddenly
One of the most noticeable signs of retinal detachment is a sudden increase in eye floaters. Unlike the occasional floaters that many people experience, these appear abruptly and in large numbers.
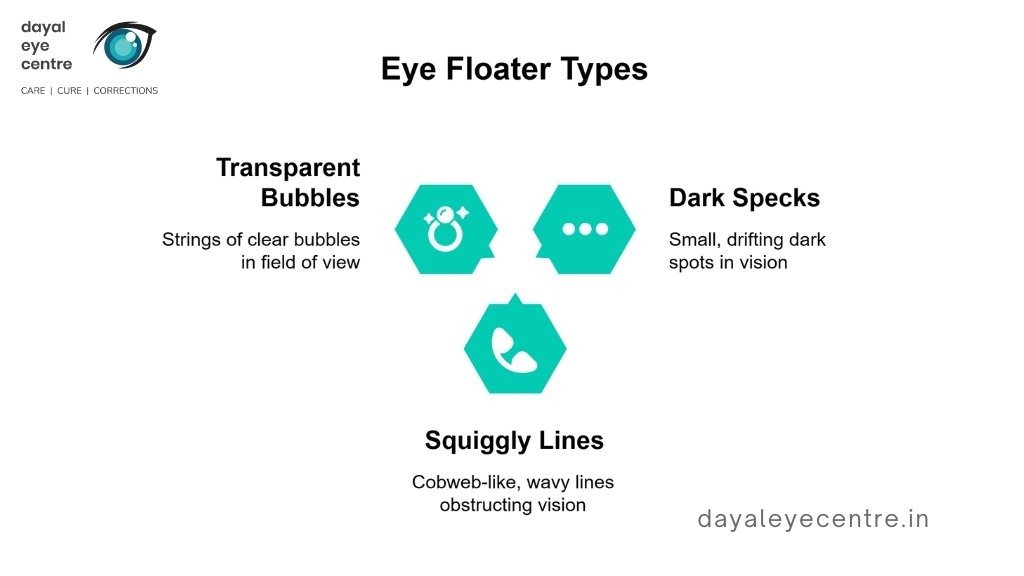
Floaters associated with retinal detachment may appear as:
- Small dark specks or dots drifting across the vision
- Squiggly lines or cobweb-like shapes
- Strings of transparent bubbles or rod-like shapes that move with eye movement
What makes these floaters concerning is their abrupt onset. While seeing a few floaters occasionally is normal, a sudden surge of new floaters requires immediate attention. In some cases, these floaters may form a ring-like pattern near the temporal side of the central vision, which can be an early warning sign before a complete detachment occurs.
Flashes of light in one or both eyes
Another telltale symptom is the sudden appearance of flashes of light, also known as photopsias. These brief flashes typically occur in the peripheral vision and may appear as bright, lightning-like streaks that recur within seconds or hours. They are often white or yellow in color and tend to be more noticeable in dark environments.
Although flashes may affect one or both eyes, they are not related to external light sources. In cases of posterior vitreous detachment, these flashes usually subside once the vitreous separation is complete and traction stops, although this process may take several days.
Dark curtain or shadow moving across vision
One of the most alarming symptoms of retinal detachment is the appearance of a shadow or curtain-like effect across the field of vision. This shadow typically begins in the peripheral vision and gradually progresses toward the center.
The curtain effect may descend from above, rise from below, or move in from either side. Many people describe it as a transparent veil partially covering their vision. Progressive darkening of peripheral vision may accompany this symptom.
Unlike many other eye conditions, retinal detachment is painless, making visual changes the primary warning signs. With prompt treatment, approximately 90% of retinal detachments can be successfully repaired. If you experience any of these symptoms—especially in combination—seek emergency medical care immediately.
How symptoms progress over time
Symptoms often begin subtly, such as with a few new floaters or occasional flashes of light. As detachment advances, symptoms typically worsen:
- Early stage: Sudden increase in floaters and flashes of light
- Intermediate stage: Dark shadows appearing in peripheral vision
- Advanced stage: Curtain-like shadow spreading toward central vision
- Late stage: Severe vision loss or blindness
If a larger portion of the retina detaches, symptoms become more pronounced. What may begin as mildly bothersome floaters can quickly progress to serious visual impairment. This progression often accelerates once the macula—the part of the retina responsible for central vision and visual precision—becomes involved.

Why symptoms can come and go
Some patients experience fluctuating signs and symptoms of retinal detachment. In the early stages, symptoms may appear temporarily and then seem to improve.
This misleading pattern can occur because:
- Small retinal tears may initially cause symptoms and then temporarily stabilize
- The brain may briefly adapt to visual disturbances
- The detachment may progress unevenly
These fluctuations should not be mistaken for healing. In most cases, they conceal ongoing, painless damage to the retina.
How long do retinal detachment symptoms last?
Without treatment, symptoms of acute retinal detachment worsen rather than resolve. Evidence shows that permanent vision loss can develop within days after detachment begins.
The timeline varies depending on:
- The location of the detachment (macular involvement leads to faster vision loss)
- The size of the detached area
- Individual factors such as age and overall eye health
Some reports suggest vision loss may occur within hours, while others indicate it may take several days. Regardless of the timeline, retinal detachment is a true ocular emergency that requires immediate medical attention. With prompt treatment, surgical repair is highly successful, with approximately 90% of cases achieving successful reattachment.
When symptoms mean an emergency
Time is critical when dealing with retinal detachment. Acting quickly can preserve vision, while delay may result in permanent blindness.
Acute retinal detachment symptoms to watch for
Contact an eye doctor immediately if you experience:
- A sudden appearance of many new floaters
- Unexpected flashes of light in your vision
- A dark shadow or “curtain” moving across your field of view
- Loss of peripheral vision or a gray curtain covering part of your sight
These symptoms are especially concerning because of their sudden onset and rapid progression. Retinal detachment is painless, making visual changes the only warning signs.
Why waiting can lead to permanent vision loss
The retina requires a constant supply of blood and oxygen to function properly. Once detached, retinal tissue begins to deteriorate rapidly. In some cases, vision loss can occur within hours.
Early treatment is highly effective—nearly 90% of patients achieve successful retinal reattachment when treated promptly. Delaying care significantly increases the risk of irreversible vision loss or blindness.
A typical progression may include:
- Minutes to hours: Initial detachment occurs
- Hours to days: Vision loss progresses
- Several days without treatment: Permanent damage becomes likely
Things to avoid with retinal detachment
If you notice symptoms or receive a diagnosis:
- Do not wait to see if symptoms improve, even if they temporarily subside
- Avoid rubbing your eyes or applying pressure
- Refrain from strenuous activities, including heavy lifting or high-impact exercise
- Do not drive yourself to emergency care, as vision changes make this unsafe
- Avoid high-velocity or contact activities during recovery, such as skydiving or contact sports
After surgery, your doctor may recommend specific head positioning—sometimes requiring you to lie face down for several days. Carefully following these instructions is essential for optimal healing.
Prompt medical attention offers the best chance of preserving vision. In cases of retinal detachment, rapid action can make the difference between recovery and permanent vision loss.

What happens after symptoms appear
Once you notice symptoms of retinal detachment, prompt medical action is critical. As with other medical conditions, successful treatment depends on accurate diagnosis and timely, specialized care.
Getting diagnosed: what to expect
Your eye doctor will begin with a dilated eye examination to thoroughly assess the retina. After applying drops to widen the pupil, the doctor will look for retinal tears, holes, or areas where the retina has separated from the back of the eye. The exam is generally painless, although some patients may find the pressure on the eyelids mildly uncomfortable.
If additional detail is needed, your doctor may recommend:
- Optical coherence tomography (OCT): Provides detailed cross-sectional images of the retina
- Ultrasound imaging: Useful if bleeding obscures the retinal view
- Fundus imaging: Offers wide-angle views of the retina
Your eye doctor will explain the findings and discuss how they influence treatment options.
Retinal detachment treatment options
If small retinal tears are detected before a full detachment occurs, treatment may include:
- Laser therapy or cryopexy: These procedures create scar tissue that seals retinal tears and helps secure the retina in place. They are typically performed in the clinic with minimal discomfort.
When a retinal detachment is present, surgery is required. When treated early, success rates approach 90%. Surgical options include:
- Pneumatic retinopexy: A gas bubble is injected into the eye to press the detached retina back into position, followed by laser or freezing treatment to seal the tear.
- Scleral buckle: A silicone band is placed around the eye to gently indent the eye wall and support retinal reattachment.
- Vitrectomy: The vitreous gel is removed and replaced with gas, air, or silicone oil to help flatten and reattach the retina.
These procedures are highly effective when performed promptly after symptoms appear, offering the best chance for vision preservation.

Surgery and recovery: what comes next
Immediately after surgery, your eye may feel sore and your vision will likely be blurry, similar to looking through a foggy window. During this period, specific positioning is crucial—especially if a gas bubble was used. You may need to:
- Keep your head in a specific position for up to seven days
- Avoid certain activities such as flying, heavy lifting, or strenuous exercise
- Use prescribed eye drops for up to six weeks
Visual recovery typically takes two to six weeks, although complete retinal healing may take several months to a year. Regular follow-up visits with your eye doctor help monitor healing and address any concerns promptly. If you experience severe pain or worsening symptoms, seek immediate medical attention.
Most patients notice significant improvement in vision, although the degree of recovery depends on how quickly treatment was initiated and how much of the retina was affected. Your eye doctor can provide guidance on what to expect during your individual recovery process.
Conclusion
Recognizing retinal detachment symptoms early can save your vision. As with many medical conditions, early detection plays a critical role in achieving the best outcome. This guide has outlined the three key warning signs of retinal detachment: sudden onset of floaters, flashes of light, and curtain-like shadows moving across the field of vision.
Time is especially critical in retinal detachment. What may begin as a few floaters can rapidly progress to permanent vision loss within days—or even hours. Prompt medical evaluation, rather than waiting to see if symptoms improve, offers the best chance of preserving sight.
The good news is that treatment is highly effective when provided early, with success rates approaching 90%. Depending on the severity, your eye doctor may recommend laser treatment for small retinal tears or surgical procedures such as pneumatic retinopexy, scleral buckle, or vitrectomy for complete detachment. Vision often begins to improve within two to six weeks, although full healing may take several months.
Vision preservation largely depends on how quickly you act. Remember these key warning signs:
- A sudden increase in floaters appearing all at once
- Flashes of light in the peripheral vision
- A dark shadow or curtain-like effect across the visual field
Contact your eye doctor immediately if you notice any of these changes. While the retina cannot heal on its own once detached, timely treatment and proper aftercare allow most patients to regain significant vision. Evidence shows that patients treated within days of symptom onset have the best outcomes.
Take these warning signs seriously—your sight depends on recognizing them and acting quickly. With prompt care and appropriate treatment, you can protect one of your most valuable senses.
FAQs
What are the primary symptoms of retinal detachment?
The main symptoms include a sudden increase in floaters, flashes of light, and a dark shadow or curtain-like effect moving across the field of vision. These symptoms often appear suddenly and may worsen quickly.
How quickly should I seek medical attention if I experience retinal detachment symptoms?
You should seek immediate medical attention if you experience any symptoms of retinal detachment. Vision loss can occur within hours or days if treatment is delayed.
Can retinal detachment be treated successfully?
Yes. Retinal detachment can be treated successfully, especially when detected early. With prompt intervention, approximately 90% of cases achieve successful retinal reattachment.
How long does it take to recover from retinal detachment surgery?
Initial vision recovery usually occurs within two to six weeks, although complete retinal healing may take several months to a year. Recovery may involve specific positioning and activity restrictions.
Are there warning signs before a full retinal detachment occurs?
Yes. Early warning signs may include an increase in floaters, brief flashes of light, or changes in peripheral vision. Prompt eye examination is essential if these symptoms occur.