Successful retinal surgery depends on matching the right procedure to your specific type of detachment. Like any other procedure in the body, retinal surgery follows clear patterns based on your unique situation.
Rhegmatogenous retinal detachment: pneumatic retinopexy or scleral buckling
Rhegmatogenous retinal detachment happens when a tear allows fluid to collect beneath your retina. Your doctor’s main goal is to find and seal all retinal breaks. Your eye surgeon will typically choose between pneumatic retinopexy, scleral buckle and vitrectomy based on your specific condition and their expertise.
Pneumatic retinopexy uses a gas bubble injected into your eye to push the retina back into place, followed by laser or freezing treatment to seal tears. This approach shows lower reattachment rates and higher recurrence than scleral buckling, but causes fewer complications afterward. The numbers tell an important story: pneumatic retinopexy achieves single-surgery reattachment in about 67% of cases compared to 95.5% with scleral buckling.
Scleral buckling involves placing a silicone band around your eye beneath the eye muscles, creating an indentation that closes retinal breaks. Though more invasive, this technique offers excellent results, with final reattachment rates reaching 100% in some studies.
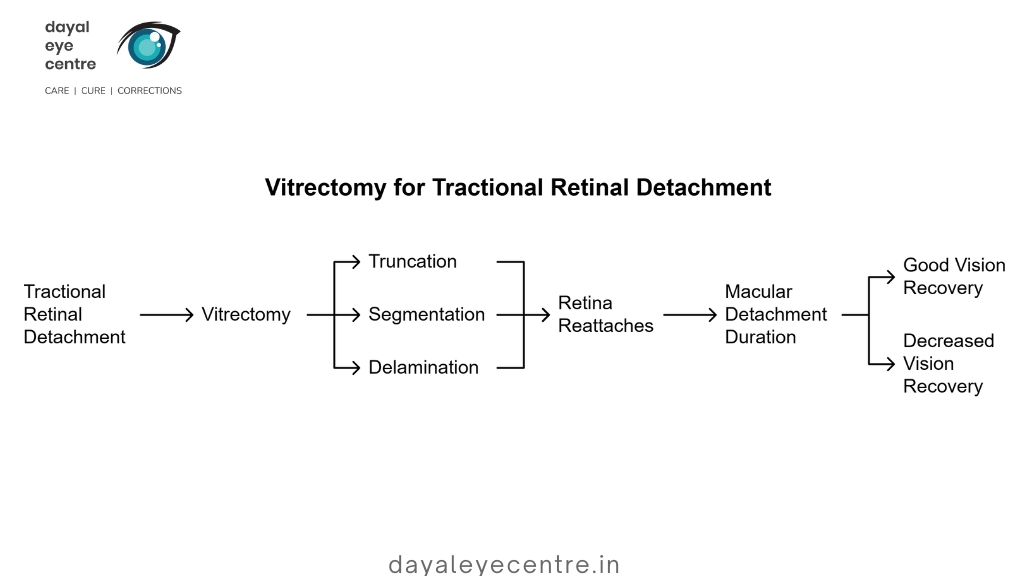
Tractional retinal detachment: vitrectomy as the primary treatment
Tractional retinal detachment occurs when fibrous membranes pull your retina away from the supporting tissue. Since the problem stems from traction rather than a tear, vitrectomy is the main treatment option.
During vitrectomy for this condition, your surgeon removes the eye’s gel-like center, relieves pulling forces by removing fibrous membranes, and allows your retina to reattach naturally. The procedure works through three key approaches: truncation (relieving front-to-back pulling), segmentation (separating abnormal blood vessel networks), and delamination (relieving traction between membranes and retina).
Time matters greatly with macular detachments. Your vision recovery chances decrease significantly the detachment lasts longer than six months, as light-sensing cells may deteriorate permanently.
Exudative retinal detachment: non-surgical management
Unlike the other types, exudative retinal detachment typically receives non-surgical treatment. This type develops when fluid builds up between your retina and the layer beneath it without any tears.
Your treatment targets the underlying cause of fluid buildup, which might include inflammatory conditions, high blood pressure, or systemic diseases. Medical approaches address these root causes rather than surgically reattaching the retina. Surgical options like scleral buckling or vitrectomy rarely come into play, and are considered only after all medical treatments have failed.
Talk with your eye doctor about which approach might work best for your specific situation. Understanding your detachment type helps you make an informed decision about treatment options.
Minimally invasive retinal tear treatments
Like any other procedure in the body, treating retinal tears requires the right approach for the best outcomes. Minimally invasive procedures effectively seal tears before they progress to full detachment. These treatments create scar tissue that prevents fluid from entering beneath the retina, stopping the detachment process.
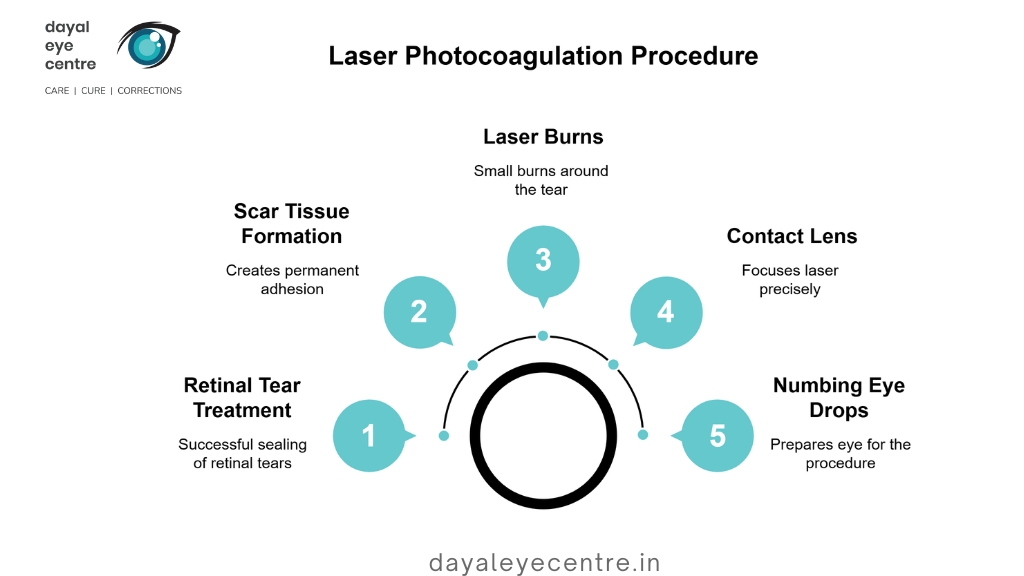
Laser photocoagulation for small retinal tears
Laser photocoagulation (also called retinopexy) treats retinal tears with success rates exceeding 90%. During this in-office procedure, your eye doctor directs a high-intensity laser beam through your pupil to create small burns around the tear. These burns form scar tissue that effectively “welds” your retina to the underlying tissue.
The procedure typically takes less than 15 minutes and involves:
- Application of numbing eye drops
- Placement of a special contact lens to focus the laser precisely
- Creation of small burns to targeted areas around the tear
You might experience bright flashes or pinprick sensations during treatment. The good news? Recovery is generally brief and involves minimal discomfort. Temporary side effects include blurred vision, floaters, flashing lights, and mild pain lasting a few hours.
Cryopexy for peripheral or large retinal tears
Cryopexy (freeze treatment) offers an alternative approach, particularly useful for peripheral tears or when a laser cannot reach the affected area. This procedure applies extreme cold to the tear site using a nitrogen-cooled probe placed on your eye’s outer surface.
The freezing process:
- Creates controlled damage that stimulates scar formation
- Seals the retinal tear to prevent fluid entry
- Secures the retina to the eyewall
Consult your doctor to determine which option is most suitable for your condition. In a comparative study, patients reported more significant post-procedure pain with cryopexy (46%) compared to laser (11%). Additionally, more patients found recovery from laser easier (52%) than from cryopexy (13%). Cryopexy remains valuable, especially for tears associated with small detachments or larger retinal breaks.
After either procedure, you will typically receive anti-inflammatory eye drops and instructions to avoid strenuous activities, such as vigorous exercise or heavy lifting, during healing. Your doctor may recommend specific positioning restrictions to facilitate proper healing of the treated area.
For both treatments, promptly addressing tears helps prevent progression to full retinal detachment, which requires more invasive surgery. Most patients see excellent results when these procedures are performed early, helping protect your vision for years to come.
In-depth look at major retinal detachment surgeries
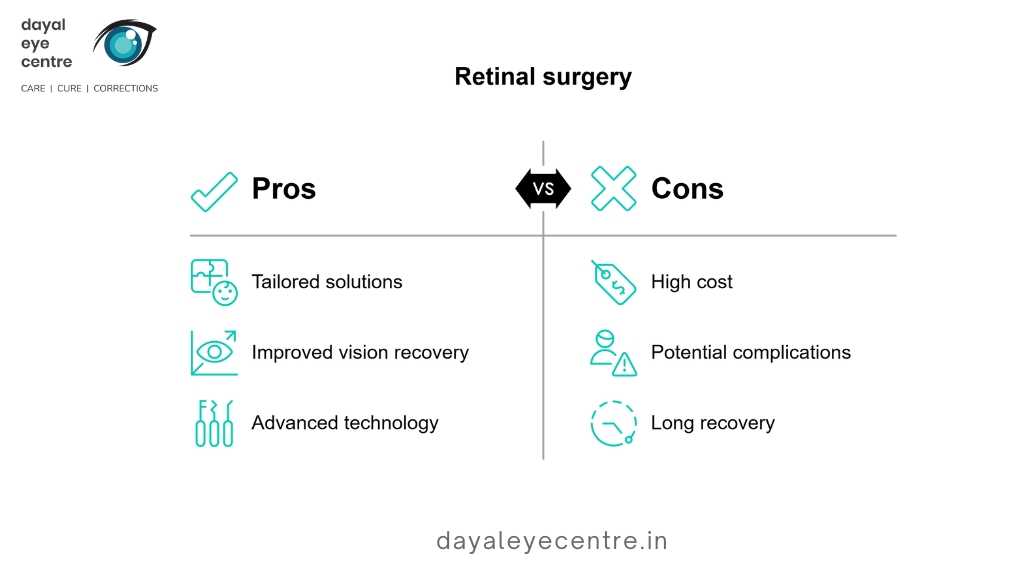
Major surgical interventions for retinal detachment have come a long way over the years. Today’s specialized approaches offer tailored solutions for different detachment scenarios, giving patients the best chance for vision recovery.
Pneumatic retinopexy: gas bubble injection and retinal sealing
Pneumatic retinopexy works well for rhegmatogenous retinal detachment, especially when breaks occur in the upper portion of the retina. During this outpatient procedure, your surgeon applies numbing eye drops, then inserts a tiny needle to remove some vitreous fluid before injecting a small gas bubble (either SF6 or C3F8). Following this, they use laser treatment photocoagulation or cryotherapy to seal the retinal tear.
The gas bubble acts like a gentle pressure pad, pushing your retina back against the eyewall and allowing natural healing to occur. This approach offers a success rate of 70-80% in appropriate cases. The good news? Pneumatic retinopexy costs approximately 25-50% less than other surgical options. After the procedure, you’ll need to maintain specific head positioning for several days to keep the bubble properly positioned against the tear.
Scleral buckle: external support for the retina
Scleral buckling creates external support for your detached retina. Your surgeon attaches a small silicone band or sponge to the outer wall of your eye (sclera). This external support indents the eyewall, pushing it inward toward the detached portion. This indentation relieves vitreous traction and helps close retinal breaks.
You’ll receive anesthesia for this procedure—either local with sedation or general. The buckle remains permanently attached to your eye unless complications develop. Studies show single-operation anatomical success rates of 70-91%, with final best-corrected visual acuity often better than with other approaches.
Vitrectomy: internal traction relief and fluid replacement
Vitrectomy addresses detachment from inside your eye. Your surgeon makes small incisions in the sclera to remove the vitreous gel. This effectively relieves internal traction on your retina. After removing the vitreous, your surgeon treats retinal tears with laser or cryotherapy.
To complete the procedure, your surgeon replaces the vitreous with gas (typically C3F8) or silicone oil to push the retina back against the eyewall. Gas gradually absorbs over 2-6 weeks, while silicone oil requires surgical removal months later.
Vitrectomy proves essential for tractional detachments, achieving approximately around 90% anatomical success. For rhegmatogenous detachments, modern vitrectomy techniques provide single-operation success rates of 83–85%.
Talk with your eye doctor about which procedure might work best for your specific situation. The choice depends on the type and location of your detachment, your overall eye health, and your surgeon’s expertise.
Preparing for and Recovering from Retinal Surgery
Like any other procedure in the body, retinal detachment surgery requires proper preparation and aftercare for successful outcomes. Understanding what happens before and after surgery helps you navigate this challenging period with greater confidence.
Pre-surgery instructions: fasting, medications, and attire
Your surgery preparation plays a crucial role in successful outcomes. Remember to fast—avoid eating or drinking anything after midnight before your procedure. For medication management, continue taking blood pressure medications with a small sip of water, but hold insulin until after surgery. Additionally, avoid aspirin or ibuprofen for 7–14 days, depending on medical advice before surgery if possible.
On surgery day, wear loose, comfortable clothing and low-heeled shoes. Leave jewelry, makeup, perfume, and hair accessories at home as these items may interfere with surgical protocols. Take note that you’ll need a designated driver since you cannot drive immediately following the procedure. Without an escort, your surgery may be canceled.
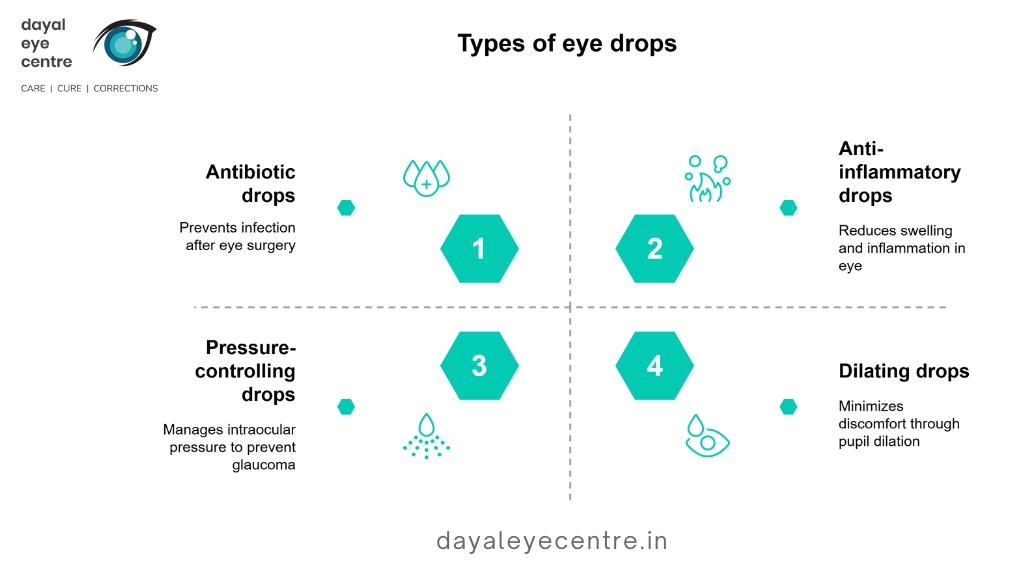
Post-surgery care: eye drops, activity restrictions, and follow-ups
Post-operative care typically involves multiple eye drops, including:
- Antibiotic drops to prevent infection
- Anti-inflammatory drops to reduce swelling
- Pressure-controlling drops to manage intraocular pressure
- Dilating drops to minimize discomfort
Activity restrictions help ensure proper healing. For the first few weeks, avoid strenuous activities, heavy lifting (over 5-10 pounds), and bending. If your procedure involves a gas bubble, you must maintain a specific head position—often face down—for several days to weeks. Importantly, altitude changes can be dangerous with gas bubbles, so avoid air travel until your doctor approves.
Follow-up appointments are essential, with the first visit typically scheduled for the day after surgery. These visits allow your surgeon to monitor healing and address any complications promptly.
Vision recovery timeline and possible complications
Your vision improves gradually after retinal surgery. You may experience blurry vision, mild discomfort, redness, and swelling initially. Visual clarity typically begins improving within 4-6 weeks. However, complete retinal healing may take up to a year or longer.
Recovery duration varies by procedure type: approximately 3 weeks or more for pneumatic retinopexy, 4 weeks or more for scleral buckle, and 4 weeks or more for vitrectomy. Throughout this period, watch for warning signs including severe pain, worsening vision, or excessive swelling—these may indicate complications requiring immediate attention.
Possible complications include eye infection, bleeding, increased eye pressure, glaucoma, cataracts, improper reattachment, or recurrent detachment. In such cases, prompt communication with your surgeon is essential for addressing these issues effectively.
Talk with your eye doctor about any concerns during recovery. Most patients experience successful outcomes when they follow their doctor’s instructions carefully. Regular check-ups help monitor your healing progress and ensure long-term vision health.
Conclusion
Retinal detachment surgery has transformed what was once a permanently blinding condition into a treatable medical emergency. Your eye doctor now has several effective options to address each type of detachment – rhegmatogenous detachments often respond well to pneumatic retinopexy or scleral buckling, while tractional detachments primarily need vitrectomy. For exudative detachments, medical treatment targeting the underlying cause usually works better than surgery.
Catching retinal tears early is crucial for your eye health. Minimally invasive procedures like laser photocoagulation and cryopexy serve as effective preventive measures with success rates exceeding 90% when applied promptly. The main surgical approaches—pneumatic retinopexy, scleral buckling, and vitrectomy—each offer distinct benefits depending on your specific situation.
Like any other procedure in the body, retinal surgery requires proper preparation and diligent aftercare. Following your doctor’s instructions about fasting, medications, eye drops, and activity restrictions helps ensure the best possible outcome. Your follow-up appointments are essential for monitoring healing and addressing any concerns.
Your vision typically improves gradually after surgery. Most patients notice clearer vision within 4-6 weeks, though complete healing takes much longer – sometimes a year or more. The numbers tell an encouraging story: most procedures achieve success rates between 70-95% , offering hope to thousands of patients annually.
Time matters most when dealing with retinal detachment. If you notice warning signs like new floaters, light flashes, or a “curtain-like shadow ” appearing in your vision, seek immediate medical attention. The difference between prompt treatment and delay can mean preserving your sight or losing it permanently.
Talk with your eye doctor about any concerns regarding retinal tears or detachment. Through proper care and early intervention, most patients enjoy restored vision and continue seeing clearly for many years afterward.
FAQs
What are the main surgical options for retinal detachment?
How long does it take to recover from retinal detachment surgery?
Are there any minimally invasive treatments for retinal tears?
What should I expect during the preparation and recovery process for retinal surgery?