Non-surgical treatments are the first line of defense against retinal diseases of all types. These therapies can treat conditions without major operations and help preserve vision through targeted approaches.
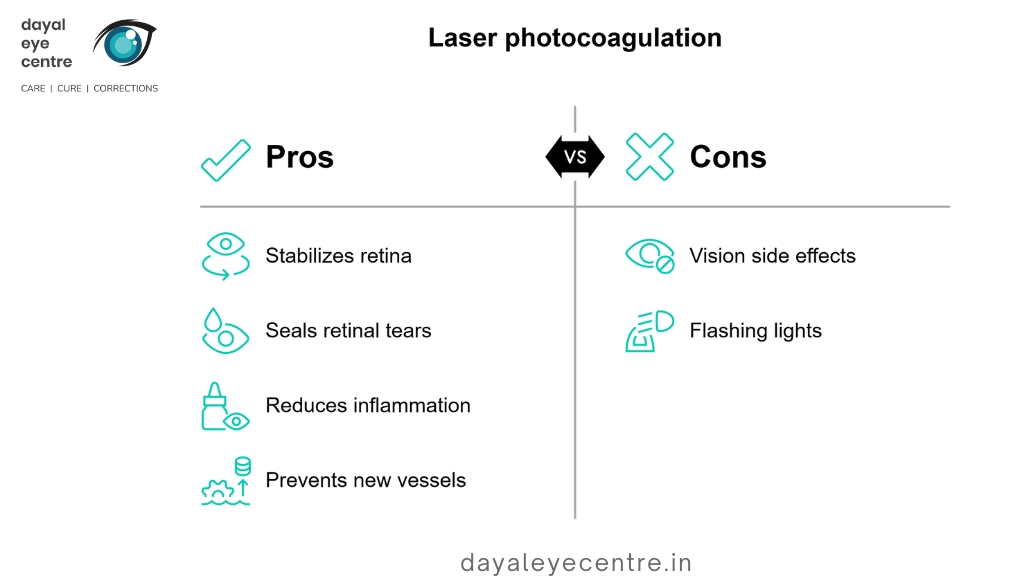
Laser photocoagulation for retinal tears and diabetic retinopathy
Laser photocoagulation is the lifeblood treatment for several retinal conditions. The procedure uses a medical laser to create microscopic burns in specific retinal areas. These burns form scar tissue that helps stabilize the retina. This treatment is mainly used to address retinal tears, diabetic retinopathy, central serous retinopathy, and macular edema.
The laser makes burns around tears in patients with retinal problems. This creates scarring that “welds” the retina to underlying tissue. The procedure is straightforward. Your doctor numbs your eye with drops and directs the laser through your pupil to seal the tear. You’ll likely see flashing lights during the treatment, which takes about 20-40 minutes.
The doctor uses scatter laser surgery (also called pan-retinal photocoagulation) to target abnormal blood vessels in diabetic retinopathy cases. The laser’s heat shrinks these vessels and stops new ones from growing. The laser treatment also helps ease inflammation, which lets the eye absorb extra fluid better.
Side effects might include reduced peripheral vision, color vision, and night vision. The benefits are substantially greater than these risks for many patients.
Cryopexy for sealing retinal breaks
Cryopexy (retinal cryotherapy) uses extreme cold to treat retinal tears and prevent detachment. This outpatient procedure applies a nitrogen-cooled probe to the eye’s exterior to freeze the area near the break. The freezing stimulates scar tissue formation and thus encourages adhesions that seal the retina and stop fluid from leaking underneath.
The procedure works like this:
- Eye dilation and application of numbing drops and local anesthetic
- Use of a specialized instrument (binocular indirect ophthalmoscope) to locate the tear
- Placement of the cryoprobe on the eye’s outer surface at the tear location
- Freezing of several areas around the break to seal it
The whole process takes about 10-15 minutes, and sealing adhesions form over 1-2 weeks. Patients should avoid heavy activities while healing. Your doctor might apply antibiotic ointment, give you an eye patch, and prescribe topical steroid drops to prevent inflammation after treatment.
Anti-VEGF injections for macular degeneration
Anti-vascular endothelial growth factor (anti-VEGF) injections have transformed treatment outcomes for wet age-related macular degeneration (AMD). These medications block VEGF, a protein that promotes abnormal blood vessel growth in the retina.
Doctors can choose from several anti-VEGF options: Lucentis (ranibizumab), Eylea (aflibercept), Beovu (brolucizumab), Vabysmo (faricimab-svoa), and off-label Avastin (bevacizumab). They inject these medications directly into the eye’s vitreous humor after using antiseptic and numbing drops.
Treatment timing depends on how each patient responds, usually every 4-12 weeks. Vabysmo can last up to four months between injections for some patients. The results are impressive – these injections improve vision in about one in three people and prevent vision loss from getting worse in nine in ten people with wet AMD.
These treatments are generally safe. Side effects might include eye redness, pain, dryness, scratches, or in rare cases, infection. A newer option, the port delivery system (PDS), uses an implanted device that slowly releases Lucentis and needs refilling only every six months.
Surgical Treatments for Retinal Detachment and Macular Holes
Doctors recommend surgery if retinal detachment or macular holes might cause permanent vision loss. The surgeon picks the best procedure based on the size, location, and how serious the condition is.
Vitrectomy procedure and use cases
A vitrectomy removes the eye’s vitreous gel to let surgeons work on the retina. The surgeon makes tiny cuts in the sclera (white part of the eye). They take out the vitreous and any scar tissue pulling on the retina. Laser photocoagulation or cryotherapy seals any tears.
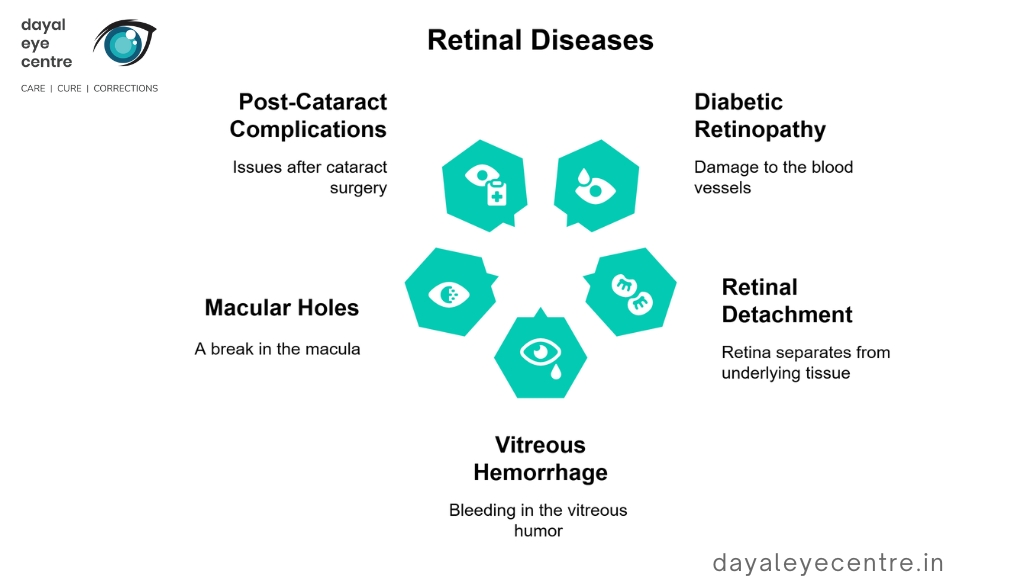
This surgery helps patients with:
- Diabetic retinopathy
- Retinal detachment
- Vitreous hemorrhage
- Macular holes
- Certain post-cataract surgery complications
The procedure reduces tension on the retina for detachments and eliminates forces that cause macular holes. The surgeon replaces the removed vitreous with saline solution, a gas bubble, or silicone oil to help flatten the retina.
Patients need to keep their face down when gas bubbles are used. This can last up to two weeks, depending on the condition. The success rate for vitrectomy exceeds 90% for macular holes, and patients get back some or most of their lost vision. The potential risks include cataracts, retinal detachment, infection, glaucoma, and bleeding.
Scleral buckling for retinal detachment
Scleral buckling is an older technique that still works well. Surgeons place a silicone band around the eye’s white part (sclera). This pushes the eye wall toward the detached retina to help it reattach.
This surgery works best for:
- Young patients
- Phakic eyes (natural lens present)
- High myopia
- Retinal detachment with breaks located anterior to the equator
The surgeon exposes the sclera and positions the buckle around the eye. They can use a complete band or sponges on both sides of the detachment. Most patients keep the silicone material permanently. The surgery usually takes 60-90 minutes.
Scleral buckling has impressive success rates of 80-90%. Notwithstanding that, doctors now use it less often as vitrectomy techniques have improved. This is in part because recovery can be more challenging.
Pneumatic retinopexy with gas bubble insertion
Pneumatic retinopexy is a simpler option that doctors can often do in their office instead of an operating room. This works best for smaller, uncomplicated detachments with superior retinal tears.
The steps include:
- Numbing the eye with local anesthetic
- Injecting a small bubble of gas (SF6 or C3F8) or air into the vitreous cavity
- Positioning the patient so the bubble pushes against the detached area
- Using laser or cryotherapy to seal retinal breaks
Patients must keep their head in specific positions for several days to keep the bubble in place. The bubble’s pressure against the eye wall helps the retina reattach as fluid underneath naturally absorbs.
Pneumatic retinopexy has a lower single-operation success rate (70-80%) compared to vitrectomy or scleral buckling (90%). This happens because the procedure leaves the vitreous gel that caused the detachment, which might create new tears.
The best candidates have a single break or several small breaks that span no more than one clock hour in the superior eight clock hours of the fundus. Patients with inferior breaks, advanced glaucoma, or proliferative vitreoretinopathy should not get this procedure.
Treatment Approaches for Hereditary and Rare Retinal Diseases
Hereditary retinal disorders are harder to treat than acquired conditions. These disorders occur due to genetic mutations that affect how the retina develops and functions. Recent scientific breakthroughs have created new hope for patients who previously had no treatment options.
Gene therapy for retinitis pigmentosa
Gene therapy has revolutionized the treatment approach for retinitis pigmentosa (RP). This breakthrough targets the mechanisms of the disease instead of just managing symptoms. Luxturna (voretigene neparvovec) remains the only FDA-approved gene therapy for RP. This treatment specifically works on the RPE65 gene mutation, which affects a subset of cases. The treatment uses an adeno-associated virus (AAV2) vector to deliver modified human RPE65 genes. This restores vitamin A metabolism in the visual cycle. Clinical trials show improved vision without serious side effects.
Scientists continue to develop new experimental approaches beyond Luxturna. Research teams focus on gene complementation for recessive RP and gene suppression techniques for dominant RP. The CRISPR-Cas9 gene editing system shows promise as another option, though getting it to work reliably in patients remains challenging. Several companies now develop treatments for X-linked retinitis pigmentosa caused by RPGR gene mutations. Some patients already show better visual field and light sensitivity.
Management of Stargardt disease and cone-rod dystrophy
Stargardt disease management focuses on controlling symptoms since no approved treatments exist. Current approaches include:
- Avoiding excess vitamin A supplements that might speed up vision loss
- Using hats and sunglasses outdoors to protect eyes
- Staying away from smoking and secondhand smoke
Research shows promise with gildeuretinol (ALK-001), a vitamin A substitute. This drug slowed retinal damage by more than 20% during a two-year study. Early-stage patients showed stable disease progression for up to seven years.
Cone-rod dystrophy also lacks curative treatments. Current management aims to maximize remaining vision through:
- Regular visual function monitoring
- Low vision service referrals
- Tinted glasses for light sensitivity
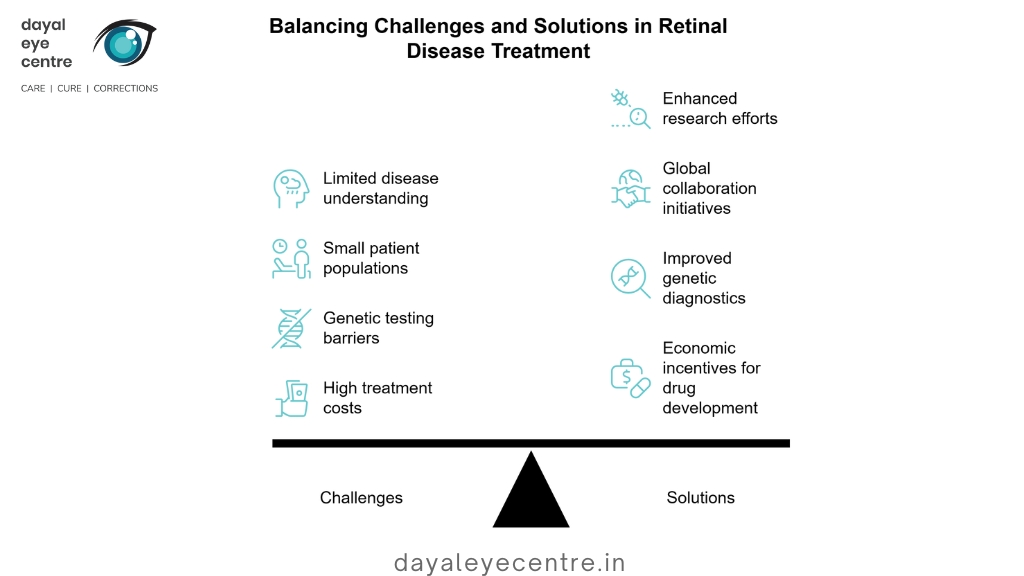
Challenges in treating rare retinal diseases
The field faces several major obstacles. Limited understanding of disease mechanisms slows treatment development. Small patient populations make it difficult to gather enough clinical data. In fact, less than fewer than 5% of rare diseases have approved treatments.
Genetic testing remains a significant barrier. About 44% of patients with inherited retinal diseases still lack a genetic diagnosis. New treatments, when available, often cost too much. Pharmaceutical companies see little financial incentive to develop “orphan drugs” for these small patient populations.
Moving forward requires worldwide cooperation. This includes building patient registries, adapting clinical trial designs, and creating economic incentives for drug development. The Foundation for Fighting Blindness Consortium exemplifies this approach. Their work helps speed up treatment development through clinical studies.
Post-Treatment Recovery and Vision Rehabilitation
Your success after retinal procedures depends on following medical guidance and getting specialized support during recovery. The healing phase after surgery plays an equally vital role as the treatment itself to achieve the best visual outcomes.
Positioning and activity restrictions after surgery
Face-down positioning (FDP) plays a significant role after many retinal procedures, especially when you have vitrectomy with gas tamponade. This position helps prevent retinal displacement and promotes healing. Your surgeon might place a gas bubble in your eye, and you’ll need to maintain this position for 50 minutes every hour. Recovery time varies based on the type of surgery. Some patients need only 24 hours of strict positioning, while others might need up to 10 days. You should avoid sleeping on your back during recovery because the bubble could touch the lens and cause the lens, causing complications.
You must avoid these activities after surgery:
- Flying in airplanes (until gas bubble disappears)
- High-altitude exposure (above 1,000 feet)
- Strenuous exercise and heavy lifting (10-20 pounds)
- Driving (your vision may be blurry)
- Swimming (for 8 weeks after surgery)
Most patients go back to work within 1-2 weeks, depending on their job requirements. People with physically demanding jobs often need more time to recover.
Use of eye drops and follow-up care
Post-operative medication usually includes antibiotic drops for one week, steroid drops for 3-6 weeks, and sometimes pressure-controlling drops. You should wash your hands really well, pull down your lower lid, and carefully put one drop in without touching your eye. Research shows that less than 10% of first-time surgery patients use their eye drops correctly.
Regular check-ups are a vital part of monitoring your healing progress and adjusting treatments when needed. Your vision will improve gradually over six months, though it might get worse right after surgery before getting better.
Vision aids and rehabilitation programs
Low vision aids are a great way to get the most out of your remaining vision if you have permanent vision loss. These tools include magnifiers, telescopes, electronic devices, and non-optical aids like lamps and large-print materials. Rehabilitation programs teach you how to adapt, and 81% of patients report an improved quality of life after completing them.
An all-encompassing approach with ophthalmologists, occupational therapists, and vision rehabilitation specialists provides the most detailed support. Healthcare teams make most referrals to rehabilitation services (41.7% of referrals), which shows how important communication between providers can be.
Preventive Measures and Long-Term Management
Prevention is the lifeblood of retinal health management that gives patients better outcomes than reactive treatments alone. Proactive strategies to preserve vision are economical solutions for retinal disease management.
Routine eye exams and early detection
Comprehensive dilated eye examinations are the first defense against retinal diseases. Regular screenings can spot conditions before symptoms appear and treatment options work best. The American Academy of Ophthalmology recommends yearly detailed eye exams for adults over 40. Patients with higher risk factors need more frequent monitoring – this includes people with family history of ocular disease, certain ethnic backgrounds, or systemic health conditions.
Vision screenings by themselves don’t work well because they create a false sense of security for people who “pass” despite having underlying vision problems. Early intervention prevents vision loss from diabetic retinopathy in 90% of cases.
Managing diabetes and hypertension to prevent retinopathy
Blood glucose control substantially reduces retinal disease development. Diabetic patients must maintain stable blood sugar through proper diet, exercise, and medication adherence. A1C testing helps track long-term glucose control while patients work with healthcare providers to set personal targets.
Blood pressure management is a vital part of retinal health preservation. Yearly check-ups with blood pressure measurements help detect high readings before retinal blood vessels get damaged. Doctors should refer patients with hypertensive retinopathy to evaluate for related conditions such as diabetes mellitus and cardiovascular abnormalities.
Protective eyewear and lifestyle changes
UV rays can harm both skin and eyes. Sunglasses with 100% UV protection and wide-brimmed hats protect eyes outdoors. Polarized lenses offer additional protection during water activities.
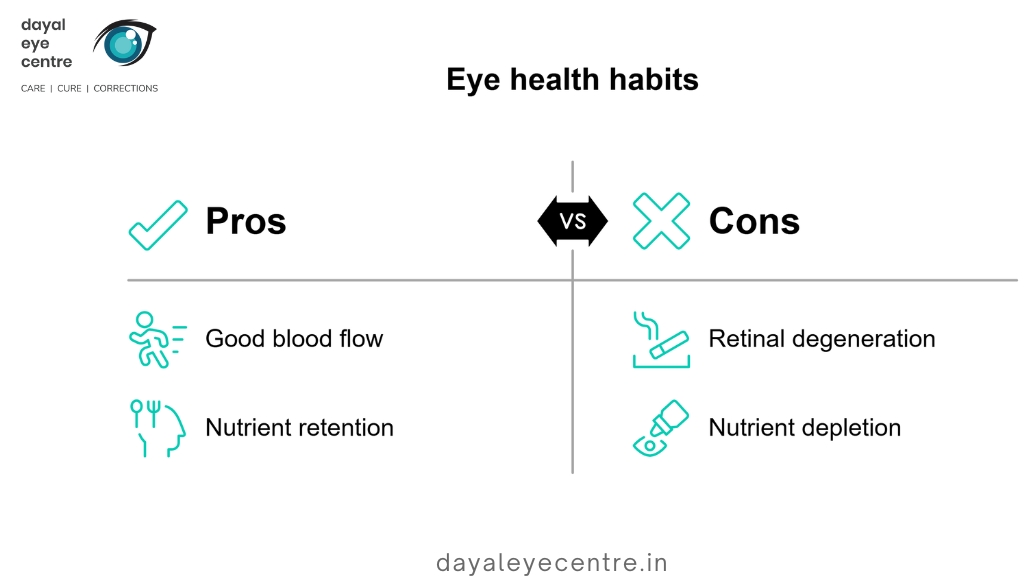
These lifestyle changes also help:
- Physical activity maintains good blood flow to the eyes
- No smoking as it accelerates retinal degeneration
- Less alcohol consumption consumption, as excessive intake can deplete essential eye nutrients
Preventive strategies combined with proper management of systemic conditions are the foundations of long-term retinal health maintenance.
Conclusion
Quality vision depends on good retinal health throughout life. This piece explores treatment options for different retinal conditions. Modern medicine provides flexible solutions for many retinal diseases. These include non-invasive laser photocoagulation, anti-VEGF injections, and advanced surgical procedures like vitrectomy and scleral buckling. On top of that, innovative developments in gene therapy bring new hope to patients with hereditary conditions like retinitis pigmentosa that were once untreatable.
Without doubt, early detection is the lifeblood of successful treatments. Regular dilated eye exams help doctors spot potential problems before symptoms show up. This allows for quick action when needed. The recovery phase after treatment is just as crucial. Patients who strictly follow positioning requirements and medication schedules see substantially better long-term results.
We have a long way to go, but we can build on this progress in managing retinal diseases. Problems are systemic, especially when you have rare conditions with few treatment options. Research keeps showing promising results, which gives patients hope. Prevention efforts work better when patients make lifestyle changes and properly manage conditions like diabetes and hypertension.
People with retinal diseases should team up with specialized ophthalmologists to find their best treatment path. Each condition needs its own approach, but the main goal remains the same – to protect vision and keep a good quality of life. Understanding your options and taking action toward retinal health gives you the ability to make smart choices about your eye care experience.
FAQs
What are some common treatments for retinal diseases?
Common treatments include laser photocoagulation for retinal tears and diabetic retinopathy, anti-VEGF injections for macular degeneration, and surgical procedures like vitrectomy and scleral buckling for retinal detachment. The specific treatment depends on the condition and its severity.
How important are regular eye exams for retinal health?
Regular comprehensive dilated eye exams are crucial for early detection of retinal diseases. They can identify conditions before visible symptoms appear, when treatment options are most effective. Annual exams are recommended for adults over 40, with more frequent monitoring for those with higher risk factors.
Can lifestyle changes help prevent retinal problems?
Yes, lifestyle modifications can significantly impact retinal health. These include maintaining a healthy diet rich in vitamins and antioxidants, regular exercise, avoiding smoking and excessive alcohol.
What is the recovery process like after retinal surgery?
Recovery after retinal surgery often involves specific positioning requirements, such as face-down positioning for certain periods. Patients may need to avoid strenuous activities, flying, and swimming for several weeks. Eye drops are typically prescribed, and regular follow-up appointments are crucial for monitoring healing progress.
Are there treatments available for hereditary retinal diseases?
While many hereditary retinal diseases lack curative treatments, advancements in gene therapy are showing promise. For example, Luxturna is an FDA-approved gene therapy for a specific type of retinitis pigmentosa. Research is ongoing for other conditions, and management often focuses on symptom control and vision rehabilitation.