Our natural lens helps us see clearly, much like a camera lens. The retina forms the innermost layer of your eye, with the specialized macula region positioned strategically for optimal vision. These structures work together but have distinct characteristics that affect how you see.
Where is the macula in the eye?
The macula in the eye occupies a precise location at the center of the retina. This yellowish spot (macula lutea) sits approximately 4 mm temporal to and 0.8 mm inferior to the center of the optic disc. Your eye doctor can observe this area during an examination – it appears darker when viewed through an ophthalmoscope due to xanthophyll pigments (lutein and zeaxanthin) that give it a characteristic yellow hue. This central positioning proves critical for detailed vision as it receives light directly from the center of your visual field.
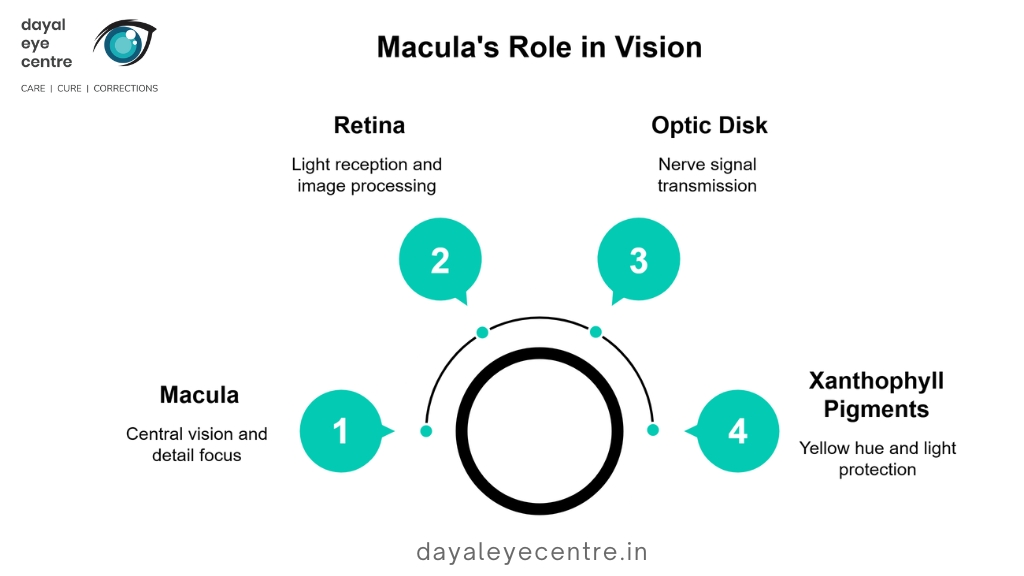
Macula anatomy: 5mm central zone of retina
The macula measures approximately 5.5 mm in diameter—less than a quarter inch across. Despite its small size, this specialized area contains several concentric zones, each serving specific functions in your vision. At its center lies the fovea, a shallow depression measuring about 1.5 mm in diameter. The fovea contains an even smaller region called the foveola (0.35 mm diameter), which sits inside a capillary-free zone. This strategic arrangement ensures nothing obstructs light from reaching the photoreceptors – similar to keeping a camera lens perfectly clean for the clearest possible image. The parafoveal area forms a 0.5 mm-wide ring surrounding these central structures.
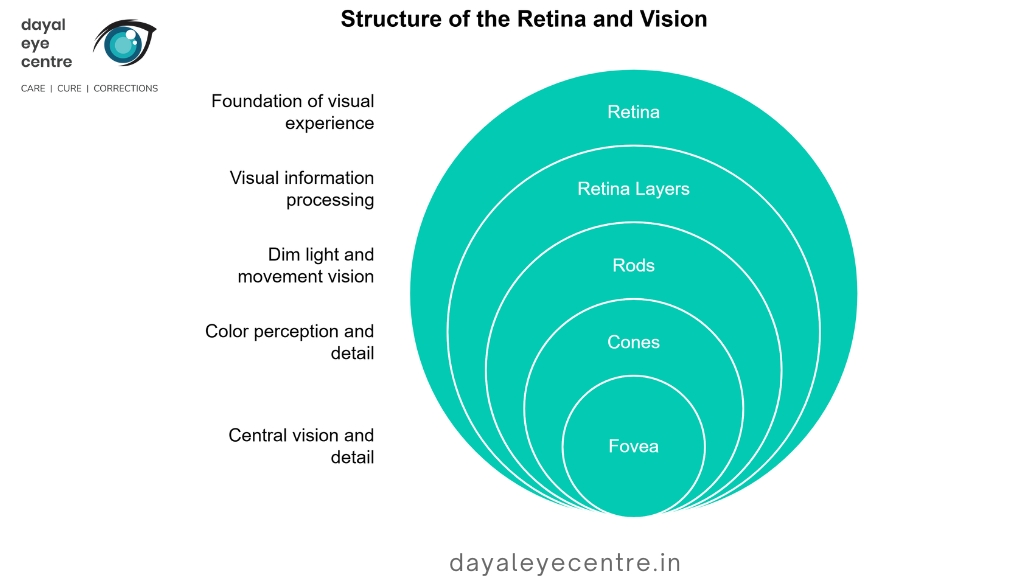
Retina eye structure: layers and photoreceptors
Your retina, though remarkably thin—approximately 0.5 mm thick—contains ten distinct layers organized in a precise arrangement. From innermost (closest to the vitreous humor) to outermost, these layers include the inner limiting membrane through to the retinal pigment epithelium. Between these boundaries lie various cellular components that process visual information before sending signals to your brain.
Photoreceptor cells—specifically rods and cones—form the foundation of your vision. The human retina contains approximately 7 million cones and between 75 to 150 million rods. Cones enable color perception and detailed vision, with their highest concentration in the macula. In fact, the key structure for detailed vision, the fovea, contains almost exclusively cones packed in a hexagonal pattern for maximum efficiency. Conversely, rods predominate in the peripheral retina, providing sensitivity to movement and vision in dim light.
Talk with your eye doctor about how these complex structures work together to create your visual experience. Understanding these components helps you make informed decisions about eye care and maintaining good vision throughout your life.
Function of Retina and Macula in Vision
Our natural lens helps us see clearly, much like a camera lens. The retina and macula work together to create the remarkable vision you experience every day. These eye structures perform different yet interconnected roles in helping you see the world around you.
Function of macula in eye: central vision and detail
Your macula primarily provides sharp central vision – what you see directly in front of you when reading this text. This tiny area lets you distinguish fine details like recognizing faces and reading small print. The fovea at the center contains the highest concentration of cone photoreceptors, making it the only part of the retina where 20/20 vision occurs.
Think of your macula like a high-definition camera lens focusing on specific details, compared to the wider-angle “standard lens” of your peripheral retina. When you look directly at an object, light focuses precisely on your macula, allowing you to see with remarkable clarity.
Retina’s role in peripheral and night vision
Beyond your macula, the peripheral retina serves two crucial functions: giving you side vision and letting you see in dim light. This larger region contains approximately 120 million rod cells, which activate primarily in low-light conditions.
While your peripheral vision lacks the sharpness of central vision, it covers a much wider area, helping you detect movement and maintain awareness of your surroundings. Studies show peripheral vision actually plays a more important role than central vision in helping you move safely, walk confidently, and keep your balance.
To test this yourself, try noticing movement at the edges of your vision while looking straight ahead. This ability helps you navigate through crowded spaces and spot potential hazards.
Macula and fovea: cone density and color perception
Your ability to perceive colors depends heavily on the macula and fovea’s high concentration of cone cells. The average peak cone density near the fovea reaches an impressive 164,000 ± 24,000 cones/mm², gradually decreasing to about 6,700 cones/mm² as you move outward to the peripheral retina. The ratio of cones to rods varies dramatically – from exclusively cones at the fovea to just 1 cone for every 23 rods in the peripheral areas.
Color vision happens through three types of cone cells containing different pigments sensitive to specific light wavelengths. Your brain interprets these as blue, green, and red. When macular disease progresses, cone cells typically weaken first, losing sensitivity to lower-intensity colors like yellows, purples and pastels ultimately leading to diminished color perception.
Like any other procedure in the body, preserving these visual functions requires ongoing care. Regular eye exams help ensure both your macula and peripheral retina stay healthy, maintaining both your detailed central vision and broader awareness of your surroundings.
Common Conditions Affecting Retina and Macula
Several conditions can affect your macula and retina, potentially causing vision loss if not treated early. Talk with your eye doctor about these common eye problems and their warning signs. Understanding these conditions helps you recognize symptoms and seek care promptly.
Age-related macular degeneration (AMD)
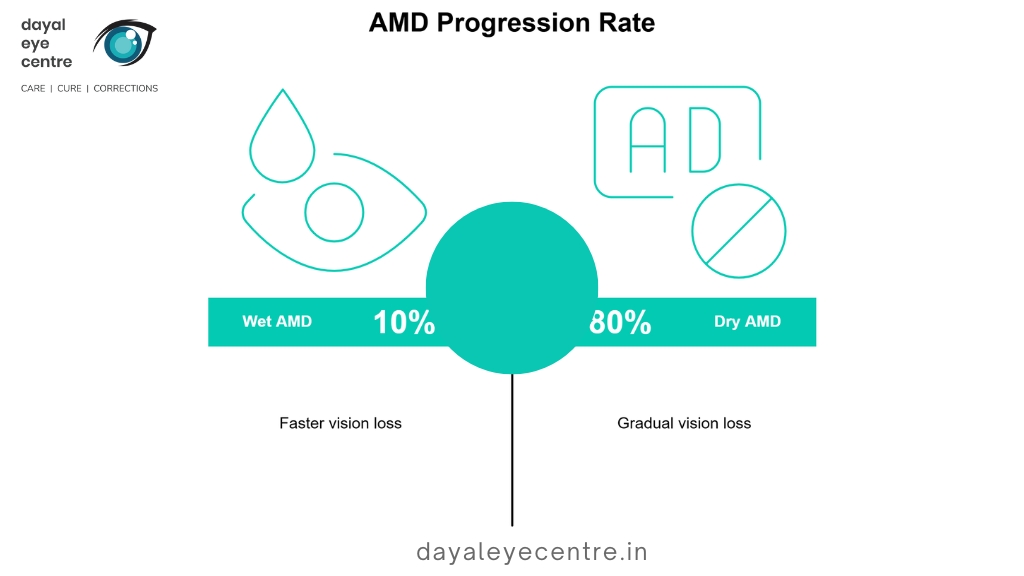
AMD represents the leading cause of vision loss in people over 60. This condition specifically targets the macula in your eye, affecting central vision while leaving peripheral vision typically intact. There are two main types:
- Dry AMD (atrophic): This more common form affects about 80% of AMD patients. It develops when tiny yellow protein deposits called drusen form under your macula, causing it to thin and dry out over time. Your vision loss generally occurs gradually, similar to a slowly fading photograph.
- Wet AMD (exudative): Though less common (about 10% of cases), wet AMD progresses more rapidly. Abnormal blood vessels grow under your retina and macula, leaking blood and fluid. This leakage causes your macula to bulge, potentially leading to faster vision loss.
Like any other procedure in the body, early detection of AMD greatly improves treatment success. Regular eye examinations help catch these changes before significant vision loss occurs.
Macular hole and macular edema
A macular hole is a small full-thickness defect in your macula. Unlike AMD, it typically occurs when the vitreous (gel-like substance filling your eye) shrinks with age and pulls on your macula, creating an opening. This condition affects about 7.8 people per 100,000 annually.
Macular edema involves fluid accumulation in your macula. This swelling occurs when damaged retinal blood vessels leak fluid or when abnormal blood vessels grow in the deep retina. The condition resembles a droplet on a screen, distorting your vision as it progresses. For diabetic patients, macular edema is the primary cause of vision loss during working years.
The good news? Treatment options for both conditions have improved significantly. With proper care, many patients maintain good vision or see improvement after treatment.
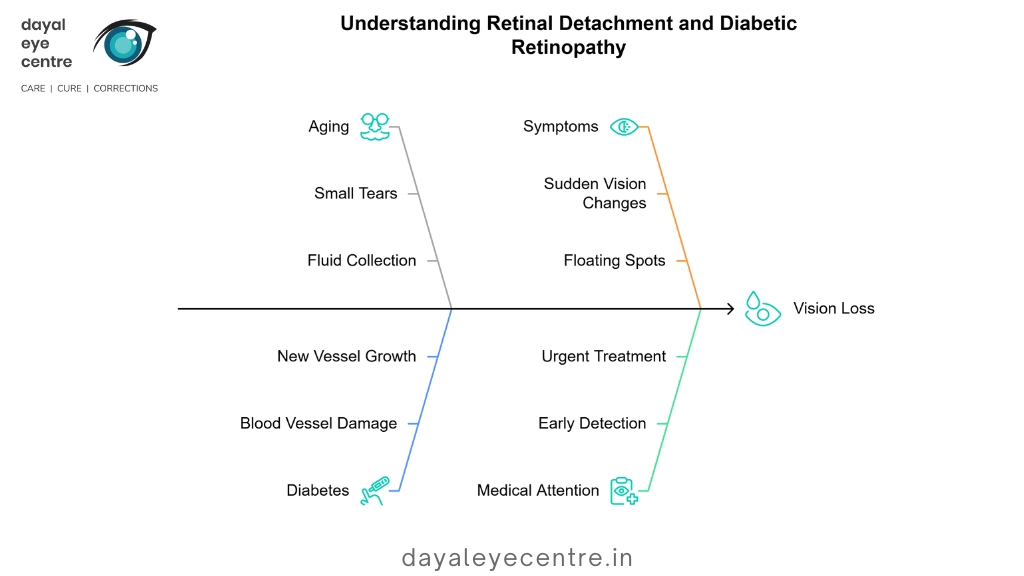
Retinal detachment and diabetic retinopathy
Retinal detachment constitutes a medical emergency where your retina pulls away from supporting tissue. The most common type typically occurs as people age when small tears allow fluid to collect behind the retina. Studies estimate annual risk at 6.3 to 17.9 per 100,000 people.
Diabetic retinopathy primarily damages blood vessels in your retina. In its early stage (nonproliferative), blood vessels weaken and bulge. As the condition advances to proliferative stage, new fragile blood vessels grow and potentially bleed. This condition represents the leading cause of blindness in working-age adults. Over time, more than half of people with diabetes develop this condition.
Your vision stability depends on catching these conditions early. If you notice sudden vision changes, floating spots, flashes of light, or a curtain-like shadow in your vision, seek immediate medical attention. These symptoms might indicate retinal detachment requiring urgent treatment.
How to Protect and Monitor Eye Health
Your macula and retina need proper care to maintain healthy vision throughout your life. Regular monitoring and preventive measures help preserve these delicate structures for years to come.
Routine eye exams and early detection
Comprehensive eye exams serve as your first defense against vision-threatening conditions. Adults should schedule check-ups every 1-2 years, even with perfect vision. If you have diabetes, annual dilated eye assessments are necessary since diabetic retinopathy often develops without noticeable symptoms. For those at higher risk of glaucoma—including Black Americans over 40, adults older than 60, and people with a family history—dilated exams every 2 years help protect your vision.
Don’t wait for your next scheduled appointment if you experience:
- Decreased vision or eye pain
- Floaters (tiny specks floating in your vision)
- Flashes of light or circles (halos) around lights
Talk with your eye doctor immediately about these symptoms, as they may indicate serious conditions requiring prompt attention.
OCT and ophthalmoscopy for macula evaluation
Modern diagnostic technologies provide detailed views of your macula and retina. Optical Coherence Tomography (OCT) creates cross-sectional images of retinal layers and is used in over 30 million eye procedures annually. During this painless 10-minute procedure, you’ll simply rest your chin in a holder while an infrared light beam scans each eye.
Ophthalmoscopy (funduscopy) allows your doctor to examine your retina, optic disc, and blood vessels directly. Before the procedure, your doctor may dilate your pupils for better visualization, which temporarily causes light sensitivity. These detailed examinations help catch early signs of macular or retinal damage before vision loss occurs.
Sun protection and managing chronic conditions
Protecting your macula functions requires consistent UV protection. Wear sunglasses that block 99-100% of UVA/UVB rays and consider adding a wide-brimmed hat for additional coverage. Choose comfort over style first—sunglasses should fit well and minimize light entering from all angles.
Managing chronic conditions proves equally important for preserving your retina and macula. Since diabetes and hypertension can damage retinal blood vessels, maintaining proper blood sugar and pressure levels protects your vision. Studies show that incorporating dark leafy greens (spinach, kale) and omega-3 rich fish (salmon, trout) into your diet supports optimal eye health.
The numbers tell a compelling story: proper protection and management of risk factors significantly reduce your chances of developing serious eye conditions. Regular check-ups help monitor these structures and address concerns promptly.
Conclusion
Understanding the difference between the macula and retina helps you make sense of how your vision works. The retina lines your entire eye wall like a camera sensor, capturing the full picture of what you see. Within this layer, the small but mighty 5mm macula area provides the sharp central vision you need for reading text, recognizing faces, and seeing color details.
Your macula contains mostly cone cells packed tightly together, especially at the fovea in its center. The rest of your retina houses primarily rod cells that help with peripheral vision and seeing in dim light. This specialized arrangement explains why conditions like AMD affect what you see straight ahead while leaving your side vision intact.
Like any other structure in the body, these delicate eye tissues need protection to function properly. Regular eye check-ups help catch potential problems before they cause significant vision loss. When your doctor examines your eyes, special imaging techniques like OCT can show the earliest signs of trouble, when treatment works best.
The numbers tell an important story: about 90% of vision loss from macular conditions could be reduced with early detection and treatment. Your vision stability depends on several factors:
- Regular comprehensive eye exams
- Proper sun protection with UV-blocking sunglasses
- Managing chronic conditions like diabetes and high blood pressure
- Eating foods rich in eye-healthy nutrients
Talk with your eye doctor about your specific risk factors and how often you should schedule check-ups. Though these structures differ in function, they work together seamlessly to create the remarkable vision you rely on daily. By protecting your eye health today, you help preserve your sight for years to come.
FAQs
-
What is the main difference between the macula and the retina?
The retina is the light-sensitive layer at the back of the eye, while the macula is a small, specialized area within the retina responsible for sharp central vision and color perception.
-
How does the function of the macula differ from the rest of the retina?
The macula, particularly its central part called the fovea, provides detailed central vision and color perception. The peripheral retina, on the other hand, is responsible for side vision and seeing in low light conditions.
-
What are some common conditions that can affect the macula?
Common macular conditions include age-related macular degeneration (AMD), macular holes, and macular edema. These conditions primarily impact central vision while peripheral vision usually remains intact.
-
How can I protect the health of my macula and retina?
Protect your eyes by wearing sunglasses that block UV rays, maintaining a healthy diet rich in dark leafy greens and omega-3 fatty acids, managing chronic conditions like diabetes, and scheduling regular comprehensive eye exams.
-
What symptoms might indicate a problem with the macula or retina
Symptoms that may indicate a problem with the macula or retina include decreased central vision, distorted vision, difficulty reading or recognizing faces, and noticing dark or blurry areas in your central vision.