Although cataract surgery is very effective, it does have disadvantages such as the risk of infection, inflammation or development of a posterior capsule opacification.
Rare complications such as retinal detachment or shifts in vision need follow-up care. Adjusting to artificial lenses can be a jarring experience for some patients at first as well.
While these advancements have led to improved outcomes, knowing about these potentialities will allow you to have more realistic expectations. It is important to discuss with your ophthalmologist to determine your individual risks and benefits before having the surgery.
Risks During Cataract Surgery
Cataract surgery is one of the most common and successful procedures done, with only a 2% chance of a complication occurring. As with any surgical procedure, there are still risks that should be taken into account. Being aware of these potential challenges will help them make the best decision possible and help set their patients up for a faster, easier recovery.
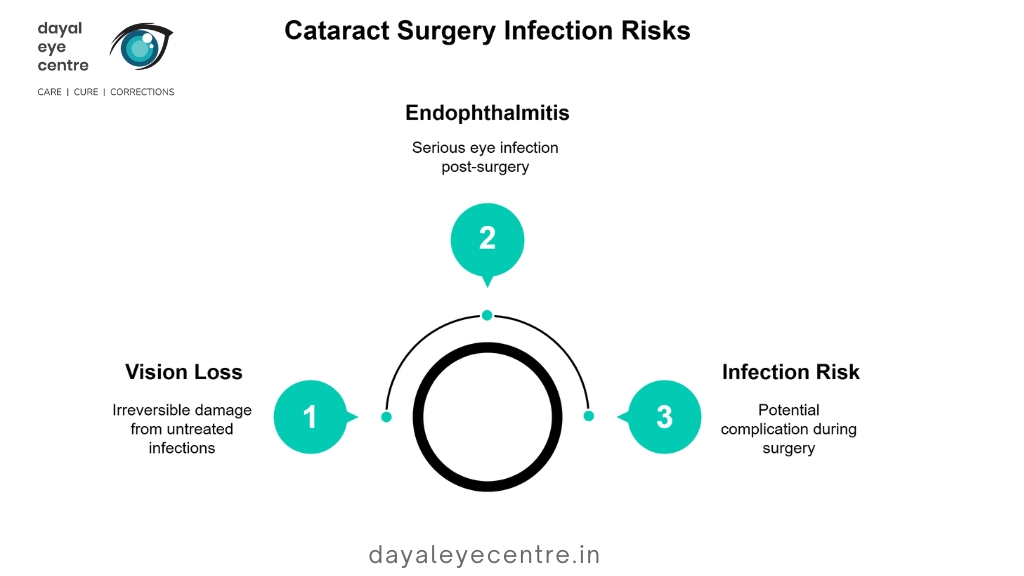
Infection Risk
Infections are one of the risks, though rare, that can happen during cataract surgery. One such infection, endophthalmitis, is especially worrisome. This serious complication, estimated to occur in 0.1% of patients, occurs when bacteria or fungi invade the eye.
Sterilization techniques during surgery can dramatically lower this risk, but maintaining oversight during the postoperative period is just as important. If you begin experiencing any symptoms like redness, pain, or sudden changes in your vision, contact your doctor immediately.
Untreated infections can lead to irreversible vision loss. Those studies show that nearly 50% of endophthalmitis cases result in permanent vision loss. This underscores the dire need for immediate action.
Bleeding Complications
Bleeding inside the eye, although rare, is another possible complication. This complication can result in delayed recovery, vision loss, or, in extreme cases, require repeat surgeries.
With careful monitoring during and after surgery, these risks are reduced. Patients with pre-existing conditions, like diabetes and high blood pressure, have to be more careful. These measures allow them to keep their bleeding tendencies well controlled.
Anesthesia Side Effects
Whether to use local or general anesthesia affects patient experience. Most side effects, like nausea or dizziness, are mild and go away on their own.
Even so, individual responses are different, so it’s important to speak to a history of medicine with your surgical team in advance. Utilizing predictive modeling through AI technology allows for more individualized anesthesia plans with a reduction of adverse effects, creating a safer procedure.
Post-Surgery Complications
While cataract surgery is one of the safest and most effective surgical procedures performed today, like any surgery, cataract surgery has risks. Even though the majority of patients heal beautifully, various complications can interfere with the healing process and the ultimate visual results. Regular follow-ups and understanding the possible issues can help you manage recovery better.
Vision Problems After Surgery
In fact, one of the most frequent experiences post surgery is blurry, or at times double vision, for the first few months of recovery. This occurs as your eye continues to heal and adapt, usually rectifying itself within eight weeks.
Not everyone will achieve perfect vision without glasses or contact lenses after surgery. If you have ongoing issues such as halos, glare, or focusing problems, bring them to your physician’s attention. As a team, you can discuss other therapies or surgical correctives.
Risk of Retinal Detachment
Retinal detachment is a rare complication, but when it occurs, it’s important to identify the signs as quickly as possible. Signs that there is a tear include sudden flashes of light, shadows in your vision or a “curtain” effect where the vision is obscured.
Immediate medical attention is critical to treat it properly and avoid permanent injury.
Swelling or Inflammation Issues
Post-operative swelling like cystoid macular edema (CME) is seen in 1%-2% of cases with contemporary techniques. Inflammation is usually short term, getting better with anti-inflammatory eye drops usually prescribed or in weeks.
Patience is important, as minor side effects including mild pain, burning, irritation, or itching are common and will typically subside over time.
Increased Eye Pressure
This includes elevated eye pressure, which can sometimes create complications after surgery, and should be carefully, regularly followed up. If left unaddressed, it can lead to a higher risk of developing glaucoma.
Consistent monitoring helps to lower the chances of increased pressure over time and their long-term impact.
Long-Term Concerns After Surgery
Cataract surgery can be a safe and effective procedure. Being aware of possible long-term issues can help you set realistic expectations and care for your eyes in the best way possible. Though complications are rare, knowing what to look for and how to approach care can better prepare you for any bumps in the road.
Secondary Cataract Formation
Commonly encountered long-term complications after cataract surgery include posterior capsule opacification (PCO) or “secondary cataract.” This condition, known as posterior capsule opacification, happens when the back part of the lens capsule (which holds the intraocular lens) clouds up.
PCO usually occurs within one to three months after surgery and can significantly affect quality of vision. Fortunately, it is easily treatable with a simple outpatient procedure known as YAG laser capsulotomy. This outpatient procedure employs a laser to make an opening in the cloudy capsule, quickly restoring clear vision.
This makes regular eye exams more important than ever to detect emerging risks and intervene before they have any significant impact on your daily life.
Dependency on Glasses or Lenses
While cataract surgery is an effective procedure that can provide major upgrades to patient’s vision, it does not guarantee full removal of corrective eyewear. Certain people might continue to need spectacles or contacts because of leftover refractive errors or special vision requirements.
Things like pre-existing astigmatism or just the way someone heals can play a factor in the outcome. Setting realistic expectations and discussing your vision correction options with your doctor ahead of time will ensure you make informed decisions.
Risk of Persistent Dry Eyes
Dry eyes are a common post-surgical woe after cataract surgery, and for many, this issue can become chronic. This is because the surgery can interfere with tear production or the eye’s natural lubrication.
Treatment varies from simple over-the-counter artificial tears to prescription treatments that are customized based on your symptoms. If you’ve developed persistent dry eyes after surgery, this could be a sign of something more serious.
Always report any pain or other issues to your eye doctor. Prompt management can go a long way in maximizing comfort and protecting your vision.
Factors That Increase Risks

Although cataract surgery is a very safe procedure with a low complication rate, some factors can increase risks for the people undergoing it. A detailed understanding of these factors can help patients make informed decisions and work collaboratively with their healthcare providers to minimize potential issues.
Pre-Existing Health Conditions
There’s no question that underlying health conditions have a huge impact on surgical outcomes. For example, diabetes affects almost 45.5% of patients with systemic comorbidities. This condition can lead to complications such as delayed healing and unsatisfactory visual outcomes.
Patients with diabetic retinopathy, glaucoma, or macular diseases have a higher risk of having an adverse post-operative visual acuity. In particular, they might have a visual acuity of less than 6/18. A comprehensive pre-operative evaluation becomes crucial to determine these hazards.
Patients need to be honest about their other medical problems. This includes considerations for hypertension, renal failure, and history of stroke, as these comorbidities can severely affect recovery and long-term prognosis. For example, a patient with a dense cataract limiting the fundal view may need more precautions to be taken during the procedure.
Age-Related Challenges
Age is an important factor as well. Such patients, particularly the elderly over 80 years, have a higher risk of complications. Studies show that individuals aged 70 and above are at greater risk of a poor visual outcome (6/18 or worse).
Aging can further decelerate the healing process, emphasizing the need for individualized surgical approaches. Surgeons will require more tailored techniques in their procedures or greater follow-up care to meet the age-specific challenges.
Surgeon’s Experience Level
In fact, the surgeon’s experience is one of the most important factors impacting success rates. For most patients, the risk of complications is less than 1%. These risks can be greatly mitigated by choosing a top-rated, experienced cataract surgeon.
Patients should be proactive, check credentials, and seek multiple opinions before moving forward. A surgeon’s familiarity with complex cases can have a significant impact on surgical results. This is particularly critical in cases that have systemic or ocular comorbidities.
Misconceptions About Cataract Surgery
Cataract surgery is the most commonly performed procedure in the world. Despite this, many still hold misconceptions about what happens after cataract surgery, recovery times, and the procedure itself. These misconceptions can color patient expectations in a way that’s not true to the actual outcomes. Addressing these myths is essential for making informed decisions about the procedure.
Guaranteed Perfect Vision Myth
Perhaps the biggest misconception about cataract surgery is that all patients will achieve 20/20 vision after the procedure. In fact, most people experience dramatic results. The outcome is less predictable if there are pre-existing eye conditions like astigmatism or macular degeneration.
The type of intraocular lens (IOL) you choose, among several other factors, play a big role in your outcomes. For instance, while a premium multifocal lens can help you depend less on glasses, it doesn’t mean you’ll never need them again. Patients need to have an open discussion about their unique eye health with their cataract surgeon to identify the possible improvements that are realistic to expect.
Misunderstanding Recovery Time
Another misconception is that cataract surgery comes with a long and painful recovery period. In fact, the majority of patients find their vision has already improved within a few days and are back to normal activity soon after.
Variables such as age, general health and ability to follow post-op directions all factor into how quickly a person will recover. Older adults with chronic health conditions can be somewhat slower to recover. They, like everyone else, can have fantastic outcomes if they listen to the science and listen to the medicine.
Overlooking Individual Variability
Each patient’s experience with cataract surgery should be unique, tailored to their age, eye health, and lifestyle needs. Though some people are thrilled with their near-perfect sight after surgery, many still need glasses for specific activities.
By knowing about this variability, you can better set realistic expectations and be pleased with the results. The most important thing is open communication with your healthcare provider to ensure the procedure is tailored to your individual needs.
Conclusion
Cataract surgery, like any operation, carries risks that you should be aware of to make an informed decision. While complications such as infection, swelling, or vision issues are rare, they can happen. Later problems, like lens dislocation or glare, can also arise but are usually fixable with quick treatment. Factors such as age, existing health issues, and not following post-operative care can increase these risks, so it’s important to stay alert.
Clear communication with your doctor helps set realistic expectations and improves outcomes. Understanding your situation allows you to weigh the positives and negatives. Always prioritize your health and consult your doctor before making any decisions. If you’re unsure, seek a specialist to clarify any confusion and guide you properly.
Frequently Asked Questions
-
What are the risks during cataract surgery?
While cataract surgery is extremely safe, potential risks include infection, bleeding, or swelling. Uncommonly, there can be retinal detachment or vision loss. Be sure to talk about these risks with your doctor prior to getting cataract surgery.
-
Can cataract surgery cause complications after the procedure?
Yes, there are complications that arise after surgery, like blurry vision, dry eyes, or inflammation. Some patients will go on to develop a condition called posterior capsule opacification (PCO) and need an additional procedure.
-
Are there any long-term concerns after cataract surgery?
Even with the long-term benefits of cataract surgery, some individuals report glare, halos, or trouble with nighttime vision. Routine follow-up visits are key to getting out ahead of any lingering complications.
-
Is cataract surgery painful?
Is cataract surgery painful No, cataract surgery is not painful. Doctors administer an injection of local anesthesia to the operative eye. You will experience some pressure during the procedure, but not pain.
-
Who is at higher risk of complications from cataract surgery?
Those with diabetes, high blood pressure, or pre-existing eye conditions are more at risk. Smokers and older adults are at higher risk for complications. Be open about your medical history with your surgeon.
-
What are common misconceptions about cataract surgery?
We found that a lot of people think cataract surgery is too risky or only appropriate for very advanced cataracts. In reality, it’s a safe, effective procedure that restores vision to 95% of patients. We know that the sooner we intervene, the better the results tend to be.
-
Can cataract surgery completely restore vision?
Cataract surgery is one of the most successful and common procedures to restore vision. It can’t remove your need for glasses entirely or take care of everything, like macular degeneration. Your physician will help you set realistic expectations.
Author
-

Dr. Sanjeev Bisla is an expert eye specialist in Gurgaon. With more than two decades of experience, he is the director and chief ophthalmologist of Dayal Eye Centre.
View all posts